Section Branding
Header Content
COVID-19 Has Pushed India's Junior Doctors To Their Limits
Primary Content
MUMBAI — Three years ago, when Shiv Joshi was studying to become a doctor at the Mahatma Gandhi Institute of Medical Sciences in central India, he had to choose a specialty. He'd been reading about the Black Death and the Spanish flu, and he wanted to learn how to track infectious diseases through triage, testing and contact tracing. So he decided to specialize in community medicine.
This was in 2018 — a century after the 1918 flu pandemic he was reading about, and two years before the coronavirus would become a full-blown pandemic in India.
"Community medicine is about preventing disease in the first place, and then also reacting to it. One of my first assignments was to investigate an epidemic of dengue fever, where an entire village had it," Joshi, 27, recalls. "But I never thought I would find myself in the middle of an actual global pandemic."
When he did, he and his fellow junior doctors — the equivalent of medical residents in the U.S. health system — were all reassigned to COVID-19 wards. Instead of shadowing more senior specialists, they often found themselves running emergency rooms and clinics and making life-or-death decisions on their own.
"All of a sudden, a lot of additional tasks and responsibilities got shifted to us," he recalls. "I lost two friends who were also doctors, and I'm routinely seeing people dying. Definitely it has been stressful."
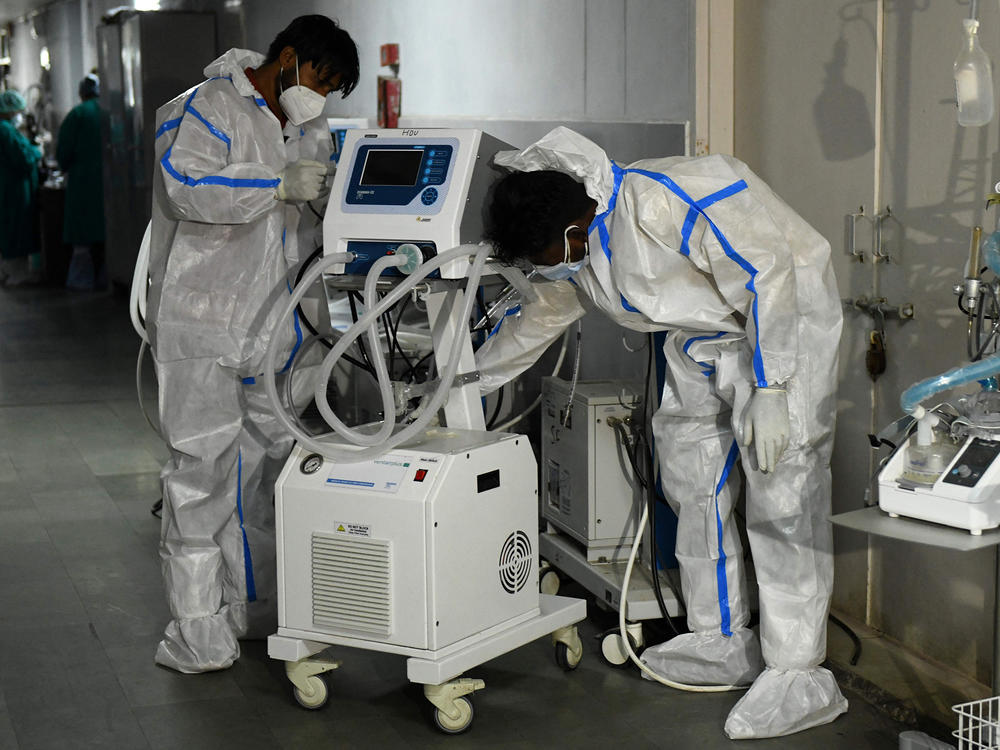
As India battles the world's biggest and deadliest COVID-19 outbreak, its junior doctors — and in some cases, even medical students — have been staffing the front lines for more than a year. They're doing the same work as more senior physicians, while those doctors oversee overflowing intensive care units and battle bureaucracy to try to fix supply chains and get deliveries of medical oxygen.
With medical board exams canceled, many junior doctors have been pressed into emergency medicine and critical care, regardless of what they studied. Working 24-hour shifts, they're often the ones who deliver bad news to grieving families and bear the brunt of anger directed at medical professionals due to shortages of oxygen and drugs.
Many have seen more death, suffering and grief in the past year than they expected in an entire career. Indian hospitals rarely provide counseling to their staff. So experts warn these junior doctors may suffer from post-traumatic stress disorder for years to come.
"What this is going to generate is a generation of doctors who are traumatized," says Devika Khanna, a psychiatrist who runs online support groups from her base in London. "That means you're reducing the capacity of medical provision for the future."
"I felt absolutely helpless"
After graduation, Joshi was assigned to a fever clinic in the same town as his medical school — Sevagram, a village of about 8,000 people. It's in an impoverished rural area, where illiteracy runs high and medical care is scant. It's also home to one of Mahatma Gandhi's ashrams.
"When the first COVID-19 case arrived in my hospital, I started realizing this problem was going to be huge," Joshi says.
He recalls one of the first times he was left in charge of the clinic. An ambulance pulled up, and the patient's family members piled out, screaming. The patient was a woman who looked extremely unwell.
"I tried to locate her heartbeat, but she was already cold — she was in shock. I had to inform my superiors. I didn't think she had a lot of time," Joshi says.
Do something, the patient's relatives pleaded, staring at him.
"But we did not have beds," he says. "Not a single bed was vacant. I mean, that was the time when I felt absolutely helpless."
He called his supervisor, but the supervisor couldn't come. All the higher-ups were too busy with other patients.
"You feel sometimes so stranded. You cannot just say that the patient is not going to survive, to their relatives, because you cannot take their hope away," he says. "Whatever the science we study, the books we read, they do not prepare us for such situations."
Joshi's patient died a half-hour later. He mustered all his strength to deliver the news to her anguished family. It would be the first of dozens of times over the year that he'd have to do so.
Threats of violence in the ER
Rimy Dey, another junior doctor, has faced similar pressures.
"The physical and mental stress is immense. In a 24-hour shift before the pandemic, we used to see 40 or 50 patients. Right now, we are seeing up to 200 — all COVID patients, all critical," Dey says. "And because of the lack of doctors, they've started assigning COVID duties to even medical students — third- or fourth-year students who have not even completed their basic medical education!"
Last month, in the wee hours of the morning, a man in his 20s stormed into Dey's emergency room at the hospital where she works in Gurugram, a suburb of India's capital, New Delhi. "Please do something, doctor! Just save my father!" the man shouted.
At the time, hospitals across the capital region were running out of medical oxygen. Hundreds of patients who might have survived COVID-19 were dying because of problems in India's medical supply chains.
The man's father was in the back of a car or an ambulance — Dey can't remember which — and was hooked up to an oxygen cylinder. But it was running low.
Her hospital had run out of beds, and there was no room for new patients.
"I had to tell him, 'Sir, this cylinder is going to run out of oxygen. We're having a severe crisis,' " Dey recounts. She gave him contacts so he could try other nearby hospitals.
"And that's when the patient's son started telling us, 'If my father dies, you will be responsible for his death! We are going to break this emergency room down.' "
Patients in their beds stared at Dey from behind their oxygen masks — wide-eyed, blinking, terrified.
"I was thinking, I did not become a doctor for this — to be scared to death while attending to patients," she says.
With help from the hospital's security guards, she was able to defuse the situation. She squeezed the man's father into her emergency room, stabilized him and eventually convinced his son to take him to another hospital with more space.
She doesn't know what happened after that. She has so many patients, she can't follow up on each one.
Afterward, Dey thought about that case for a long time. It troubled her, because the son was right: She had been responsible for his father's care in a health system that was collapsing.
And it often feels like it's collapsing on her shoulders: "I'm checking a patient, declaring a patient dead and then going back [home] and crying for hours," she says.
Lack of support for young doctors
Dey says she often feels angry at India's government for leaving junior doctors overworked and lacking in support. Even before the pandemic, India invested less in public health — just above 1% of its gross domestic product — than most other countries. (The U.S. spends nearly 18% of its GDP on health, though most of that is private, not public, investment.)
India's government was blindsided by COVID-19's second wave. In January and February, daily caseloads hit record lows. By early March, the country's health minister declared that India was in the "endgame" of the pandemic. Extra wards were disassembled, and lockdown restrictions eased.
But new virus variants were circulating — even as Prime Minister Narendra Modi presided over huge political rallies and failed to curb a massive Hindu pilgrimage that drew millions of devotees to the banks of the Ganges River.
In April and May, India broke records for the most coronavirus cases and deaths in the world, straining its already understaffed and underfunded health system.
NPR asked Dey and Joshi if their facilities — Dey's urban and private, Joshi's rural and public — offer them counseling or mental health support. Both say they are unaware of any such resource. In any case, both say, they have no time to devote to therapy.
"Most of the time, it falls on us junior doctors to support one another," Joshi says.
He and his fellow junior doctors try to allay one another's fears. They've been learning on the job while watching their own families and friends fall ill — and worrying about their own health.
He and his colleagues belong to a WhatsApp group where they send each other words of encouragement. But the group is also a place where they share grim news stories about fellow junior doctors who've taken their own lives. It seems there are stories like this every month, Dey says.
More than 500 doctors have died in India's second COVID-19 wave, according to the Indian Medical Association, which does not specify how many of those were suicides.
Experts warn the stress these junior doctors describe may have a lasting impact.
Khanna, the London-based psychiatrist, says post-traumatic stress disorder is often compounded by the sense the junior doctors share that government action could have prevented the worst and India's second COVID-19 wave didn't have to be this bad.
"When there's a natural disaster, then trauma is obviously huge. But the PTSD from a man-made disaster is much greater, because there's that sense that people weren't looked after," Khanna says. "If God or the universe did it to you, it's different to if human beings did it to you. It feels so much more personal."
"I have grown ahead of my years"
After more than a year of treating COVID-19 in the rural fever clinic, Joshi recently tested positive for coronavirus antibodies. It means he probably had the virus at some point and didn't realize it. Knowing he's already survived the virus is a relief, he says. He'd spent a year wondering whether he would be able to get a bed in his own hospital if he fell gravely ill.
"That saddens me the most," he says. "How can you work in a hospital, in a pandemic, at your fullest, knowing that if you get infected, there might be nothing available to you?"
Dey's father and brother, back in her home state of Assam, got sick with COVID-19 this winter, and she wasn't able to travel to see them. They've since recovered. But sometimes it feels like only her fellow junior doctors can really understand what she's going through.
"We've seen a lot more than we should have at our age. When I see old friends from school, they're actually enjoying the lockdown! They're enjoying being at home," she says with a laugh. "And here I am, seeing a lot of death every day and coming back to my room and crying. I think I have grown ahead of my years."
She says her hair is already turning gray. She's 28. But she has no plans to leave medicine.
NPR producer Sushmita Pathak contributed to this report from Hyderabad, India.
Copyright 2021 NPR. To see more, visit https://www.npr.org.