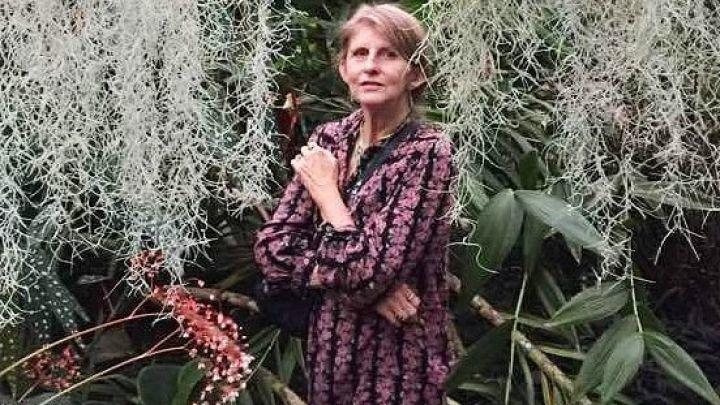
Caption
Margot Judd of Douglasville was 40 years old when she learned that a blood transfusion that she’d had in the 1980s made her sick. She died in 2019 at age 68 from complications of hepatitis C, which is now curable in the early stages.
Credit: Family photo



