Loading...
Section Branding
Header Content
Omicron may be less severe in South Africa. That may not be the case for the U.S.
Primary Content
It's been about a month since scientists first detected the highly mutated coronavirus variant dubbed "omicron."
Since then, scientists have come to learn that omicron spreads faster than the delta variant and is the quickest-spreading variant the world has yet faced. It also has a huge ability to bypass immune protection and cause breakthrough infections.
The big open-ended question right now centers on omicron's severity: Does omicron cause milder disease, compared to previous variants? Does it thereby lower the risk of severe disease and hospitalization?
There's no doubt everyone wants this to be the case. And some recent data out of South Africa sure makes it look like that might be the case. Researchers there have found that South Africans infected with omicron are, on average, less likely to end up in the hospital, and they also appear to recover more quickly from illness, compared to the other variants.
However, as many scientists have been pointing out, that evidence from South Africa could be misleading. The omicron variant may end up acting differently in the U.S.
Omicron brings less severe disease in South Africa
First, let's look more closely at all that good news from South Africa. Some of the best data comes from a large study, presented to the press on Tuesday, from the South African Medical Research Council in collaboration with Discovery Health, a large health insurance company.
Their study looked at more than 200,000 COVID cases in South Africa during a delta-driven surge in September and October, and the beginning of the omicron-driven surge in November, as that variant began increasing rapidly in South Africa. About a quarter of the people in the study already have a chronic illness, putting them at higher risk of severe COVID.
What the researchers found is quite hopeful: The risk of hospitalization for adults dropped 30% during the early days of the omicron surge from the levels seen there in September and October.
"The hospital admissions during omicron, standing at 58 per 1,000 infections, are the lowest of the four COVID waves, and one-third of what we experienced during the delta surge," Discovery Health CEO Ryan Noach said in a presentation on Tuesday.
On average, the infected people who did end up in the hospital weren't as sick, he noted. Fewer of these coronavirus patients required oxygen and ventilation, and the proportion who required intensive care, or ended up in the ICU, dropped to about 13% from 30%, Noach and his colleagues found.
On top of that, people seemed to recover more quickly from omicron compared to delta, whether they were in the hospital or not, Noach said. Outside the hospitals, many people recovered after only three to four days. "We believe there is hope that the severity is lower," he said.
But while the researchers presented these promising findings to the press this week, they kept reminding the audience over and over again of an important caveat: This data doesn't take into account prior exposure to the virus.
"Therefore, we must exercise caution interpreting these severity findings," Noach said repeatedly.
South Africans have built up significant COVID immunity
As a country, South Africa had already gone through three massive COVID surges, as vaccination rates there remained low, compared to the U.S. and Europe.
So, while only about a quarter of South Africans had been vaccinated when omicron finally arrived, the vast majority of residents had likely already been infected with previous variants of SARS-CoV-2. (Scientists have predicted this based on the excess mortality rate observed in the country through the pandemic.) Given this history, scientists say most South Africans already probably had some level of immune protection generated by these prior infections.
"Thus, omicron enters a South African population with considerably more immunity than any prior SARS-CoV-2 variant," concluded Dr. Roby Bhattacharyya, an infectious disease specialist, and epidemiologist William Hanage in a recent paper published online.
In other words, there are very few South Africans who have never been exposed to the coronavirus — either through a vaccine or a natural infection.
That means the omicron infections happening in South Africa aren't, for the most part, primary infections, but rather secondary infections, also known as reinfections.
Here's the thing about secondary infections from SARS-C0V-2: They tend, on average, to be milder, scientists have found. For example, a study published last month in the New England Journal of Medicine found that if you survive the first infection, it reduces the risk of severe illness from a second infection by about 90%.
And thus, even before omicron hit South Africa, the population as a whole had built up a significant amount of immunity to COVID-19. A large proportion of people who were once — early in the pandemic — at high risk for severe disease, are now probably at a lower risk.
This background level of immunity within a population muddies the water when trying to figure out if omicron causes more mild illness, according to Ryan Noach and his colleagues at Discovery Health. Given South Africa's current level of immunity, you would expect more mild illness – even if the omicron variant is actually just as dangerous as its predecessors.
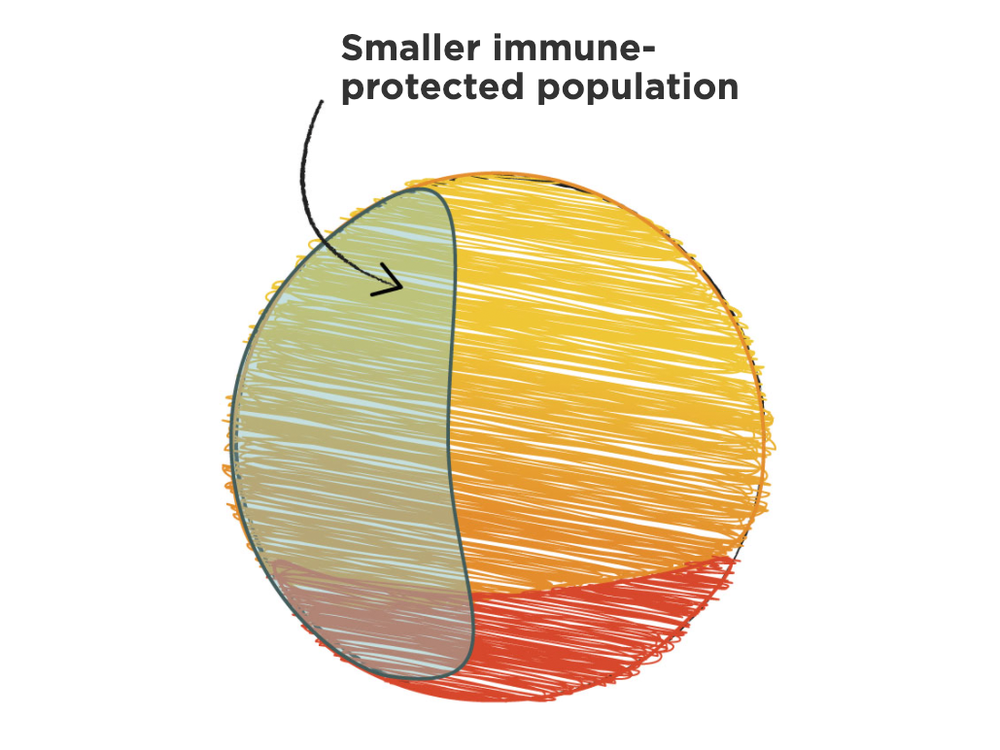
To put it another way, this background immunity only makes omicron appear less harmful. But what happens when omicron makes its way into a population without that background level of immunity?
Bhattacharyya and Hanagepoint out another confounding factor: it's still early days. During the initial stages of a surge, the lag between cases and hospitalizations can make a new variant seem less severe — especially if the variant is also spreading much faster than previous variants, as omicron is doing now.
How much immune protection do Americans have against omicron?
In the U.S., health officials don't have a precise understanding of how many people are "naive" – as scientists call it – to SARS-CoV-2. That is, there isn't a reliable estimate for how many people have neither had a vaccination nor had a bout of COVID, leaving them at higher risk for hospitalization and severe disease than those who have some immunity to the virus.
Right now, a little over 62% of Americans have had two doses of the vaccine. That will still offer some protection against severe disease with omicron, scientists in South Africa predict. But that leaves about 125 million Americans who don't have that vaccine-induced protection.
What about the percentage of Americans who have some immune protection from a prior infection? That's tougher to estimate, says Maciej Boni, an epidemiologist at Pennsylvania State University, because many mild or asymptomatic infections go undetected or unreported. But a recent study by computational biologists at the University of Texas at Austin estimated that about 20% of Americans had been infected with COVID from the start of the pandemic, through August, 2021.
Taken all together, the data suggest that at minimum, 20% of Americans still have had neither a vaccine, nor a prior infection. That's about 66 million people who have immune systems that are completely "naive," as scientists term it, when it comes to exposure to SARS-CoV-2.
Right now, the Centers for Disease Control estimates cases of omicron are doubling every two or three days in the U.S., and predict that in a few weeks, it could be the dominant variant across the country.
The 66 million Americans people who are naive to SARS-CoV-2 are the people for whom the omicron variant poses the greatest risk. These are the people who are most likely to end up in the hospital during an omicron surge. These are the people for whom a "less severe" variant in South Africa, may actually be a "severe" variant in the U.S.
Copyright 2021 NPR. To see more, visit https://www.npr.org.