Section Branding
Header Content
Why humans are losing the race against superbugs
Primary Content
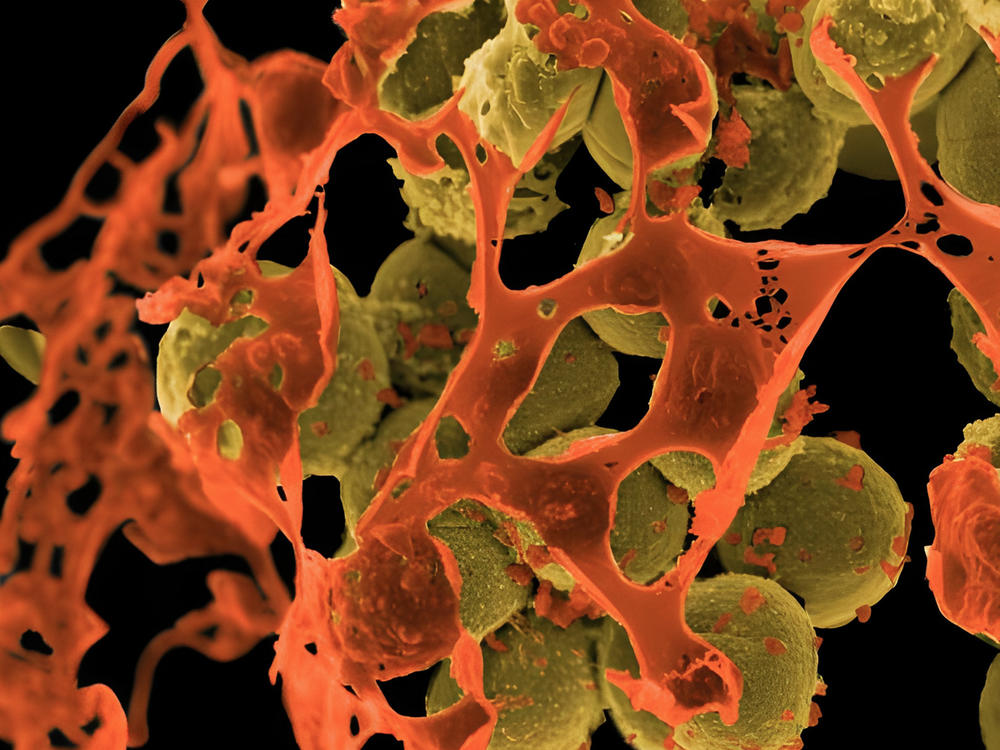
Drug-resistant bacteria — also known as superbugs — are on the rise globally, and they're now killing more people each year than either HIV/AIDS or malaria. And low- and middle-income countries are being hit the hardest by the rise in antibiotic-resistant infections.
"That resistance out there is actually now one of the leading causes of death in the world," says Dr. Chris Murray, the director of the Institute for Health Metrics and Evaluation. Murray is one of the authors of a new study, published in the medical journal The Lancet, that finds that in 2019, drug-resistant infections directly killed 1.2 million people and played a role in 5 million more deaths worldwide. Murray and his colleagues set out to quantify how much of a problem antibiotic resistance is globally, and they found that bacteria are mutating to evade antibiotics at a pace far faster than many researchers had previously forecast.
These deadly new strains of bacteria are causing untreatable blood infections, fatal pneumonia, relentless urinary tract infections, gangrenous wounds and terminal cases of sepsis, among other conditions.
The conventional wisdom used to be that the failure of antibiotics was a "First World" problem. But Murray says this new study shows it happening all over the world.
"In the past, we all thought that you had to be rich enough to use a lot of antibiotics inappropriately to have this problem," he says. "But that's not the case."
The researchers calculate that deaths caused directly by antibiotic resistance are the highest in sub-Saharan Africa, causing 24 deaths per 100,000 population annually, compared with an average fatality rate of 13 per 100,000 in high-income countries. Australia has the lowest mortality rate globally from antibiotic resistance, at 6 deaths per 100,000.
Latin America is right in the middle. But Fiorella Krapp Lopez, an infectious disease physician in Lima, Peru, says being in the middle is still quite bad.
"We do have a very high frequency of resistance to different types of antibiotics, first line and second line [antibiotics]," Krapp says. "And the problem has been increasing in the last years."
She says antibiotic resistance is affecting every level of health care in Peru.
"Unfortunately, I think it's everywhere. We are seeing it in the community with infections that used to be very simple to treat, like urinary infections," she says. Physicians are seeing minor wounds that in the past may have needed only a bandage but now are turning into multidrug-resistant infections. "And we also see it in very sick patients with bloodstream infections or very severe pneumonia. So unfortunately, it's across the full spectrum of bacterial infectious diseases right now in Peru," she says.
Krapp was one of dozens of researchers around the world who contributed to the new Lancet report. She provided data specifically on drug resistance in Peru.
She says there are many reasons that this problem is harder to address in low- and middle-income countries.
First, antibiotics are often readily available to anyone without a prescription. Misuse and overuse of these drugs fuels mutations in bacteria, leading to more resistance.
Second, the systems to flag and test for potentially drug-resistant infections are not as robust as in some wealthier countries.
Third, low- and middle-income countries in general report higher rates of infections in hospitals than high-income countries do, and those infections are more likely to be drug resistant.
Fourth, while some new, more powerful antibiotics are being developed, lower-income countries are still dependent on older, cheaper, less-effective drugs.
Krapp says the COVID-19 crisis exacerbated all of these problems in Peru. And while it's too early to tell, she worries that the coronavirus pandemic has led to a significant increase in drug resistance.
"First, there was a lot of antibiotic use during the pandemic," she says. As the COVID-19 crisis pounded Peru, many people who contracted the virus did not want to go anywhere near the overcrowded hospitals, so they self-medicated at home.
"It is still very easy to get antibiotics in the local pharmacy without a prescription," Krapp notes. "Unfortunately, more than 70, 80% of [COVID-19] patients that arrived to the hospital were already using antibiotics at home."
They believed the drugs would aid in their recovery. But antibiotics target bacteria and wouldn't be of much help against a coronavirus.
This scenario may be one of the reasons that Peru has had the world's highest per capita death rate from COVID-19. At times, hospitals and clinics were barely able to function as they were inundated with patients.
"We believe that a lot of the high COVID mortality that we had in Peru was due to secondary infections acquired in the hospitals rather than just by COVID-19," Krapp says.
Whether or not that happened is hard to say. Monitoring for antibacterial resistance in Peru — and in many other lower-income countries — is limited during the best of times but especially unlikely when hospitals are overflowing with COVID-19 patients.
"During the pandemic, the hospitals were overloaded. A lot of patients went into ICUs that were understaffed. That was just the perfect storm to have a very high transmission of these [drug-resistant] pathogens," she says.
It's unclear if that was happening because as health care workers were simply trying to keep COVID-19 patients breathing, testing bacterial samples for resistance fell low on the priority list.
Krapp says that overall she's very concerned that bacteria are evolving and learning how to evade what had been some of the world's most powerful drugs.
"We are in a race, and these bacteria are moving faster than we are," she says. "They are becoming resistant much faster than we humans are able to create new antibiotics and make those antibiotics accessible to the most vulnerable populations."
Copyright 2022 NPR. To see more, visit https://www.npr.org.