Section Branding
Header Content
TB is good at resisting antibiotics. Here are some new ideas to outsmart the bacteria
Primary Content
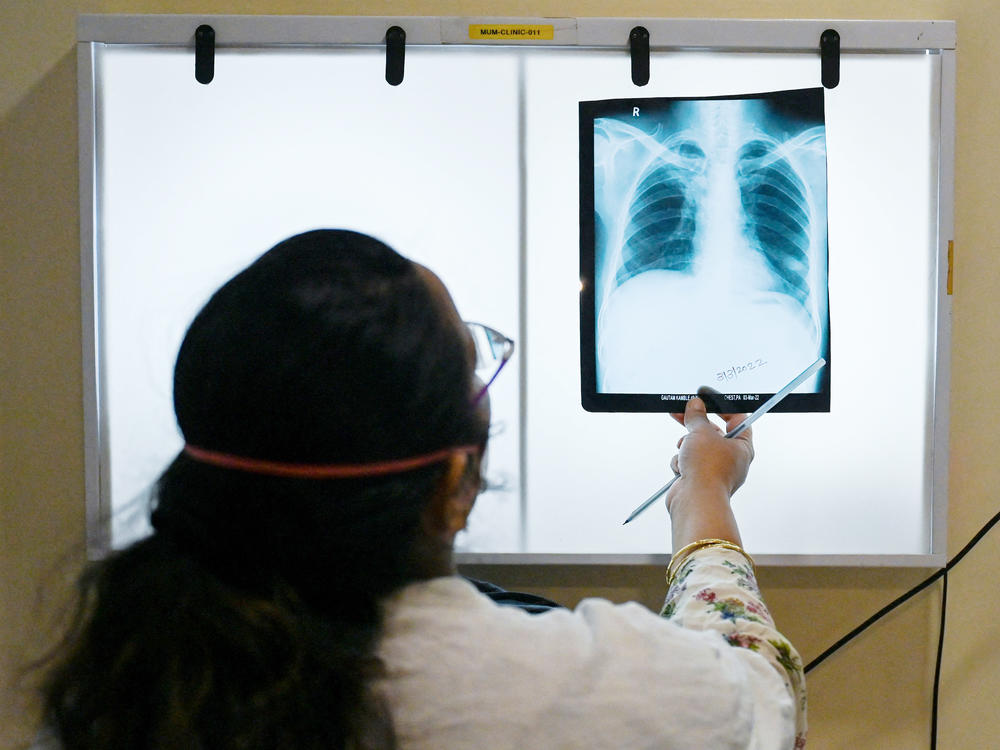
Tuberculosis, or TB, is a bacterial infection of the lungs that can be fatal. The World Health Organization estimates 1.5 million people died of the disease worldwide in 2020. It remains a persistent foe in large part because the bacteria can mutate and evolve to develop resistance to our antibiotics (often within a patient, which can lead to relapse).
Now, in a pair of studies published this week in PLoS Biology, scientists have found an array of new genes associated with that drug resistance, hinting at how we might battle the disease going forward.
The researchers analyzed bacterial samples from more than 12,000 patients across Asia, Africa, South America and Europe, examining their resistance to 13 first- and second-line antibiotics — a "comprehensive [analysis] of the genetic variation in the bacteria" that cause tuberculosis, says Zamin Iqbal, a computational biologist at the European Molecular Biology Laboratory's European Bioinformatics Institute and co-author of the two studies.
One thing they learned is that some mutations may cause a little resistance while others may cause a lot. That is, the situation is more complex and nuanced. To come up with that finding, instead of asking whether the bacteria were resistant or not — a simple up or down vote — they looked to see just how much drug was required to kill the bug. In other words, in some cases where a mutation causes low-level resistance, higher doses of the drug initially prompting the resistance may well vanquish the bacteria. And with this approach of progressively doubling the dose until you see the bacteria collapse, "you can explain more drug resistance than we ever realized," says Iqbal.
In addition, the team was able to surface not just common mutations that scientists know about that lead to resistance but also less common ones that can be harder to spot.
And if you know which resistance-causing mutations are present in a particular strain of the TB-causing bacteria in a patient, that could determine the course of treatment, says Iqbal. Already, DNA sequencing can let clinicians know if four of the first-line antibiotics are likely to work in treating TB. The new studies out this week expand on this strategy by considering additional drugs.
In the future, Iqbal explains that a health-care professional could prescribe a customized cocktail of effective antibiotics. One approach would be to find two antibiotics that the bacteria can't be resistant to at once – so if the bacteria develops resistance to one, it would be susceptible to the other. "If you can find pairs of drugs like that," Iqbal says, "they're the perfect weapons to use."
That's what Iqbal hopes lies ahead. "We're still in the foothills of properly understanding" how it all works, he says.
Dr. Lucica Ditiu, executive director of the U.N.'s Stop TB Partnership, says that the new studies represent "significant steps toward enhancing our knowledge on the association of drug resistance and genetic mutation in the TB bacteria." Current methods for determining which antibiotics will be most effective against a patient's particular TB sample are insufficient and take too long, she says.
But because it's challenging to look at a patient's tuberculosis bacteria for all possible mutations, the findings of this work will take time to reach clinics and TB wards. In the meantime, the researchers have made the data from these studies publicly available in an effort to accelerate the fight against the disease. "It's a much bigger project than we can do on our own," Iqbal says.
Copyright 2022 NPR. To see more, visit https://www.npr.org.