Section Branding
Header Content
New Clues To ALS And Alzheimer's Disease From Physics
Primary Content
The same process that causes dew drops to form on a blade of grass appears to play an important role in Alzheimer's disease and other brain diseases.
The process, known as phase transition, is what allows water vapor to condense into liquid water, or even freeze into solid ice. That same sort of process allows brain cells to constantly reorganize their inner machinery.
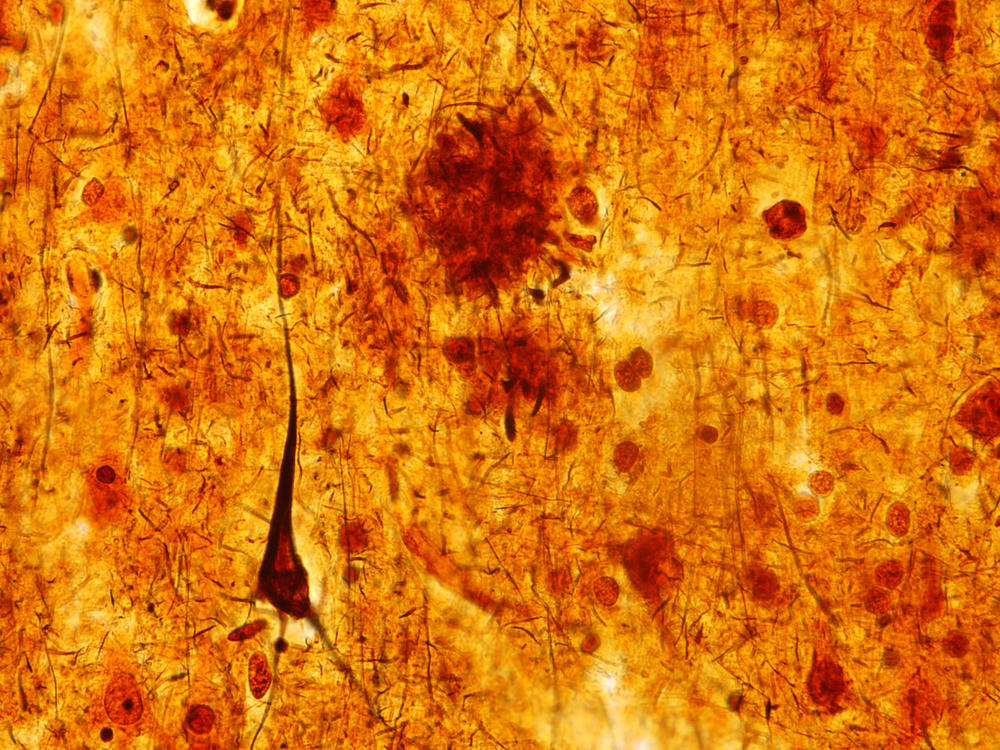
But in degenerative diseases that include amyotrophic lateral sclerosis, frontotemporal dementia and Alzheimer's, the phase transitions inside neurons seem to go awry, says Dr. J. Paul Taylor, a neurogeneticist at St. Jude Children's Research Hospital in Memphis, and an investigator with the Howard Hughes Medical Institute.
This malfunctioning prompts the interior of the cell to become too viscous, Taylor says. "It's as if you took a jar of honey [and] left it in the refrigerator overnight."
In this sticky environment, structures that previously could nimbly disassemble and move around become "irreversibly glommed together," says Clifford Brangwynne, a professor of chemical and biological engineering at Princeton University and an investigator with the Howard Hughes Medical Institute. "And when they're irreversibly stuck like that, they can no longer leave to perform functions elsewhere in the cell."
That glitch seems to allow toxins to begin to build up in and around these dysfunctional cells, Taylor says — including the toxins associated with Alzheimer's and other neurodegenerative diseases.
The science behind this view of brain diseases has emerged only in the past decade.
In 2009, Brangwynne was part of a team that published a study showing that phase transitions are important inside cells — or at least inside the reproductive cells of worms.
"Originally, there was not a lot of traction for that idea," Brangwynne says. "Then — around about 2015 — people started to suddenly pay a lot of attention."
By that time, Taylor, too, had stumbled upon phase transition via a very different path.
As a practicing neurologist and geneticist at the University of Pennsylvania, he'd seen himself as a sort of medical detective.
"Typically the most oddball diseases that didn't fit into another category would wind up in my clinic, which I loved," he says.
One disease in particular caught Taylor's attention.
"We had been tracking a number of families that had an unusual degenerative illness," he says. "It was kind of a blend of a dementia and ALS."
Patients developed the mental problems of dementia as well as the muscle weakness of ALS, or Lou Gehrig's disease.
Taylor figured there must be a genetic explanation. But at the time — the late 2000s — he had no easy way to study his patients' DNA.
"So I collected those [DNA samples] and hung on to them for years," he says. "And then the world changed around me."
Seemingly overnight, it became feasible to sequence a person's entire genome. Taylor saw an opportunity.
"I dug those DNAs back out of the freezer," he says. "And we were fortunate enough to find the genetic basis for the disease in these families that I had known for, at that point, a decade."
What Taylor found was gene mutations that caused abnormal phase transitions in cells. And he found evidence of similar mutations in other neurodegenerative diseases.
This research earned Taylor the 2020 Potamkin Prize, a big deal in Alzheimer's research. And it got a lot of biotech companies thinking about ways to fix problems with phase transitions inside cells.
"I think it's probably safe to say that you'll see some of these types of therapies within the next couple of years," Taylor says.
Brangwynne says neurodegenerative diseases are an appealing target because the physics behind the problem is now clear, and because cells already contain mechanisms to regulate phase transition.
Inside a healthy nerve cell, he says, many molecules act a bit like people socializing.
"Something like at a party, where we've got little clusters of people hanging out and having nice conversations," he says. "They're free to come and go as they please."
That can change, though — at a party or inside a brain cell.
"What happens in neurodegenerative disease is that the 'people' are irreversibly stuck together — they can't leave," Brangwynne says. "This is the Hotel California of biomolecular interactions."
But Brangwynne says that doesn't have to be the case.
In the lab, at least, experimental drugs and genetic tweaks have been used to unstick these molecules.
That could lead to new treatments for neurodegenerative diseases, Brangwynne says. And the ability to correct aberrant phase transitions may also be useful for other illnesses, including certain cancers, he says.
"It's very clear that this principle is at play in many, many diseases," Brangwynne says.
The startup Dewpoint Therapeutics hopes to develop phase-transition treatments for both cancer and neurodegenerative diseases. Late last year, Dewpoint, which is based in Boston and Dresden, Germany, signed a $100 million deal with the pharmaceutical giant Bayer.
Copyright 2020 NPR. To see more, visit https://www.npr.org.