Section Branding
Header Content
Across The COVID-Ravaged South, High-Level Life Support Is Difficult To Find
Primary Content
Hospital discharge day for Phoua Yang was more like a pep rally.
On her way rolling out of Centennial Medical Center in Nashville, she teared up as streamers and confetti rained down on her. Nurses chanted her name as they wheeled her out of the hospital for the first time since she arrived in February with COVID-19, barely able to breathe.
The 38-year-old mother is living proof of the power of ECMO — a method of oxygenating a patient's blood outside the body, then pumping it back in. Her story helps explain why a shortage of trained staff who can run the machines that perform this extracorporeal membrane oxygenation has become such a pinch point as COVID-19 hospitalizations surge.
"One hundred forty six days is a long time," Yang says of the time she spent on the ECMO machine. "It's been like a forever journey with me."
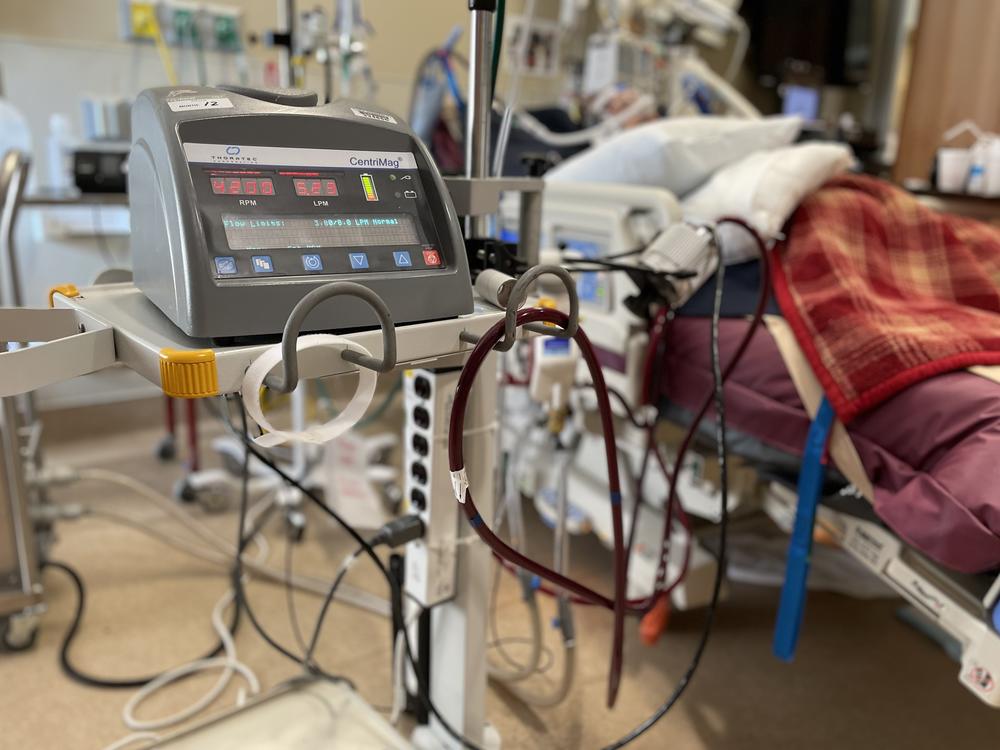
For nearly five months, Yang had blood pumping out a hole in her neck and running through the rolling ECMO cart by her bed.
ECMO is the highest level of life support — beyond a ventilator, which pumps oxygen via a tube through the windpipe, down into the lungs. The ECMO process, in contrast, basically functions as a heart and lungs outside the body.
The process, more often used before the pandemic for organ transplant candidates, is not a treatment. But it buys time for the lungs of patients who have COVID-19 to heal. Often they've been on a ventilator for a while. Even when it's working well, a ventilator can have its own side-effects after prolonged use — including nerve damage or damage to the lung itself through the excessive air pressure.
Doctors often describe ECMO as a way to let the lungs "rest" — especially useful when even ventilation isn't fully oxygenating a patient's blood.
Many more people could benefit from ECMO than are receiving it, which has made for a messy triaging of treatment that could escalate in the coming weeks as the delta variant surges across the South and in rural communities with low vaccination rates.
ECMO is labor intensive and expensive
The ECMO logjam primarily stems from just how many people it takes to care for each patient. A one-on-one nurse is required, 24 hours a day. The staff shortages that many hospitals in hot zones are facing compound the problem.
Yang says she sometimes had four or five clinical staff members helping her when she needed to take a daily walk through the hospital halls to keep her muscles working. One person's job was just to make sure no hoses kinked as she moved, since the machine was literally keeping her alive.
Of all the patients treated in an ICU, those on ECMO require the most attention, says nurse Kristin Nguyen who works in the ICU at Vanderbilt University Medical Center.
"It's very labor-intensive," she tells us one morning, after a one-on-one shift with an ECMO patient who had already been in the ICU three weeks.
The Extracorporeal Life Support Association says the average ECMO patient with COVID-19 spends two weeks on the machine, though many physicians say their patients average a month or more.
"These patients take so long to recover, and they're eating up our hospital beds because they come in and they stay," Nguyen says. "And that's where we're getting in such a bind."
Too few hospitals are equipped to handle such patients
It's not that there aren't enough ECMO machines to go around or the high cost — which is estimated at $5,000 a day or significantly more, depending on the hospital.
"There are plenty of ECMO machines — it's people who know how to run it," says Dr. Robert Bartlett, a retired surgeon at the University of Michigan who helped pioneer the technology.
Every children's hospital has ECMO, where it's regularly used on newborns who are having trouble with their lungs. But Bartlett says prior to the pandemic, there was no point in training teams elsewhere to use ECMO when they might only use the technology a few times a year.
It's a fairly high risk intervention with little room for error. And it requires a round-the-clock team.
"We really don't think it should be that every little hospital has ECMO," Bartlett says.
Bartlett says his research team is working to make it so ECMO can be offered outside an ICU — and possibly even send patients home with a wearable device. But that's years away.
Only the largest medical centers offer ECMO currently, and that's meant most hospitals in the south have been left waiting to transfer patients to a major medical center during the recent pandemic surge. But there's no formal way to make those transfers happen. And the larger hospitals have their own COVID patients eligible for ECMO who would be willing to try it.
"We have to make tough choices. That's really what it comes down to — how sick are you, and what's the availability?" says Dr. Harshit Rao, chief clinical officer overseeing ICU doctors with physician services firm Envision. He works with ICUs in Dallas and Houston.
There is no formal process for prioritizing patients, though a national nonprofit has started a registry. And there's limited data on which factors make some patients who have COVID-19more likely to benefit from ECMO than others.
A surge of younger patients has increased the demand for ECMO
ECMO has been used in the United States throughout the pandemic. But there wasn't as much of a shortage early on when the people dying from COVID-19 tended to be older. ECMO is rarely used for anyone elderly or with health conditions that would keep them from seeing much benefit.
Even before the pandemic, there was intense debate about whether ECMO was just an expensive "bridge to nowhere" for most patients. Currently, the survival rate for COVID-19 patients on ECMO is roughly 50% — a figure that has been dropping as more families of sicker patients have been pushing for life-support.
But the calculation is different for the younger people who make up this summer's wave of largely unvaccinated COVID-19 patients in ICUs. So there's more demand for ECMO.
"I think it's 100% directed at the fact that they're younger patients," says Dr. Mani Daneshmand, who leads the transplant and ECMO programs at Emory University Hospital.
Even as big as Emory is, the Atlanta hospital is turning down multiple requests a day to transfer COVID-19 patients who need ECMO, Daneshmand says. And calls are coming in from all over the Southeast.
"When you have a 30-year-old or 40-year-old or someone who has just become a parent, you're going to call. We've gotten calls for 18-year-olds," he says. "There are a lot of people who are very young who are needing a lot of support, and a lot of them are dying."
Even for younger people, who tend to have better chances on ECMO, many are debilitated afterward.
Laura Lyons was a comedian with a day job in New York City before the pandemic. Though just 31 years old when she came down with COVID-19, she nearly died. ECMO, she says, saved her life. But she may never be the same.
"I was running around New York City a year and half ago, and now I'm in a wheelchair," she says. "My doctors have told me I'll be on oxygen forever, and I'm just choosing not to accept that. I just don't see my life attached to a cord."
Lyons now lives at her parents' house in central Massachusetts, and spends most days doing physical therapy. Her struggle to regain her strength continues, but she's alive.
Some families take their plea for ECMO public
Since it's kind of the wild west to even get someone an ECMO bed, some families have made their desperation public, as their loved one waits on a ventilator.
As soon as Toby Plumlee's wife was put on a ventilator in August, he started pressing her doctors about ECMO. She was in a north Georgia community hospital, and the family searched for help at bigger hospitals — looking 500 miles in every direction.
"But the more you research, the more you read, the more you talk to the hospital, the more you start to see what a shortage it really is," he says. "You get to the point, the only thing you can do is pray for your loved one — that they're going to survive."
Plumlee says his wife made it to sixth in line at a hospital 200 miles away — Centennial Medical Center where Phoua Yang was finishing her 146-day ECMO marathon.
Yang left with a miracle. Plumlee and their children were left in mourning. His wife died before ever getting ECMO — a few days after turning 40.
This story was produced as part of NPR's partnership with Kaiser Health News and Nashville Public Radio.
Copyright 2021 NPR. To see more, visit https://www.npr.org.