Section Branding
Header Content
For two years, this Washington island has grappled with the long reach of COVID
Primary Content
It didn't take long for the pandemic to arrive on Whidbey Island. That pastoral slice of the Pacific Northwest meanders through the upper reaches of Puget Sound, coming within just 30 miles of downtown Seattle. It was this corner of the country that alerted Americans to the reality that a virus doesn't abide by international borders and a global pandemic had made landfall in the U.S.
The very first confirmed case of COVID-19 in the U.S. was here, in Washington state. And by early March of 2020, the virus had torn through a nursing home in a quiet suburb on the eastern edges of Lake Washington. That outbreak marked some of the very first known U.S. deaths of the pandemic. As ambulances shuttled those patients to a nearby hospital, the rest of the country was left to wonder: When would those scenes of panic and disease reach their hometowns, their hospitals, their parents, siblings and spouses?
Not long after, the virus had caught a ride to Whidbey Island, home to about 70,000 residents. And there, too, the daily rhythms of life changed almost instantly. The place enjoys a strange kind of isolation. It runs 55 miles north to south and is counted among the longest islands in the U.S. On the map, Whidbey could almost pass as a peculiar peninsula, suspended in the jumble of waterways and small islands that dot the region.
In reality, though, it is severed from the mainland. A strait, known as Deception Pass, runs between Whidbey and neighboring Fidalgo Island, which nearly touches the eastern shores of the Sound. Other than by air, there are only two ways on and off: by taking a short ferry ride; or braving a two-lane, steel bridge that soars 180 feet above the water before depositing travelers in a forest nearly two hours north of Seattle.
The story of the coronavirus pandemic is often told in extremes. An avalanche of patients overwhelming a hospital in New York. Refrigerated trucks serving as makeshift morgues in Texas. Bodies stacked to the ceiling at funeral homes in Florida.
That is not Whidbey Island.
As with everywhere, people there have lost family, friends, jobs and futures. But those who care for the community talk of a more subtle, persistent erosion, one that's jeopardizing the well-being of the most vulnerable.
WhidbeyHealth Medical Center seems to embody this unfolding crisis. With 25 beds, the island's only hospital is on tenuous footing. The pandemic only compounded years of financial stress. It's a familiar predicament for health care in rural America. Losing the hospital would be losing a lifeline. Patients would have to travel farther for life-saving care. Others would be left behind. This is what's at stake for Whidbey Island in this precarious moment.
When the virus first washed over the island, photojournalist Lynn Johnson was there. Now, two years and a million deaths later, we go back to see how the island and its people are finding their way through the pandemic that has quietly but indelibly altered the place they call home.
Tony Johnson, Longtime Island Resident
At first, Tony Johnson thought he'd emerged from a deep, deep sleep.
He didn't know that just a week earlier the doctors had told his wife he'd likely never wake up. He didn't know the nurses had played rock and roll for him while he was unconscious. He didn't know that he'd soon need to relearn how to breathe and swallow. And he had no idea that COVID-19 would take even more from him than it already had during those nine days on a ventilator.
When he first moved to Whidbey Island more than two decades ago, Johnson says it was a low-key place, populated by a bunch of "old hippies." That appealed to him. So did the waterfront, the arts and crafts fair and the street dance that was held every year. Some of that charm is very much alive there, but over time Johnson felt a shift. New people arrived, and so did developers. It became more expensive. His family could only get by thanks to thrift stores and Walmart.
Eventually, he and his wife moved to Oak Harbor. It's a military town on the north end of the island with a humming naval base. After years of steady work, Johnson lost his job at the bank.
"Suddenly you find yourself isolated in a small community and there is no work," he says. "That made it really tough."
Just a few years ago, their mobile home was condemned. The water system was contaminated. Johnson had even fallen ill from an E. coli infection. Later, his wife fell through the decaying porch floor. She had to be rescued by a neighbor.
In March of 2020, the virus gained a foothold in the Whidbey nursing home, where Johnson was living at the time. Soon he was one of the very first COVID-19 patients on the island. He was high risk, diabetic and over 60. Somehow he survived, though he'd come off the ventilator with blood clots in his feet.
He was moved off the island as he recovered. But his wounds weren't healing well – weeks went by without anyone tending to them. Infection set in, consuming his toes and feet. A vascular surgeon was able to restore blood flow in one leg. The other one could not be salvaged, though. "They said, 'You can either die from gangrene or we can amputate your leg,'" Johnson recalls. "It was not that hard of a decision."
Johnson says he doesn't miss the island so much anymore. By then, his home there was gone, just a graveled lot now. Still, he talks with remarkable ease about all that COVID-19 took from him. There are even some surprising flashes of humor. "You can bury it deep or you can just let it out," he says. "It's better to let it out, so it doesn't eat you up the same way."
Delores Jetton, hospice aide
There's only one time when Delores Jetton refers to her work as a "job." And it's when she tells you, "I love my job." In her warm voice, she speaks of it more like a devotional practice — one she can only perform with deliberate hands and unceasing curiosity. She bathes people, people who are dying, at home, in hospice. "Some make me laugh, some make me cry," Jetton says. "I still love them all the same." Working with the aging has always appealed to her. After all, they have the best stories. Her mantra? All you have to do is ask them one good question. "You better make it count," she chuckles.
The intimacy of her work underwent a strange transformation during the pandemic. Suddenly, she was shrouded, head to toe with a gown, gloves and mask. People would sometimes ask to see her face. She'd finish bathing them, step outside and peel off her layers. Then she'd stand at their window and smile. Others don't care about seeing her face. They simply want to feel her hand on their arm or have her rub their feet.
Jetton has spent many years on the island. She moved there from Maryland because her daughter was stationed at the base there. Her daughter left, but she stayed. The weather was nice and so was the connectedness, a sense that everyone knows each other even if they're from different sides of the island: "I have yet to run into any rude people."
Before Jetton enters the home of a new patient, she pauses and says a prayer. She'll tell you the hands she uses to wash people, people who are on the edge of life, don't quite belong to her. "I ask the Lord to lead me, to make me sensitive to their needs and show me what you want me to do with them," she says.
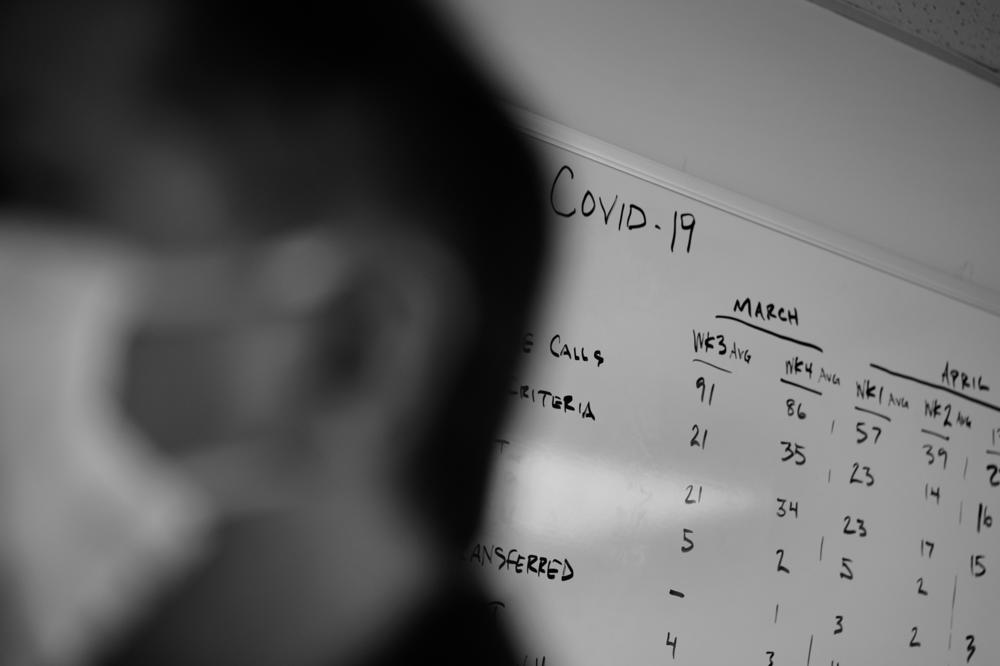
Tabitha Sierra, nurse manager
Tabitha Sierra does well during a crisis. She had studied public health in California, and then went on to train as an emergency trauma nurse. Eventually, she'd found her way to Whidbey to take a job at the hospital. She liked the idea of her kids growing up on the island.
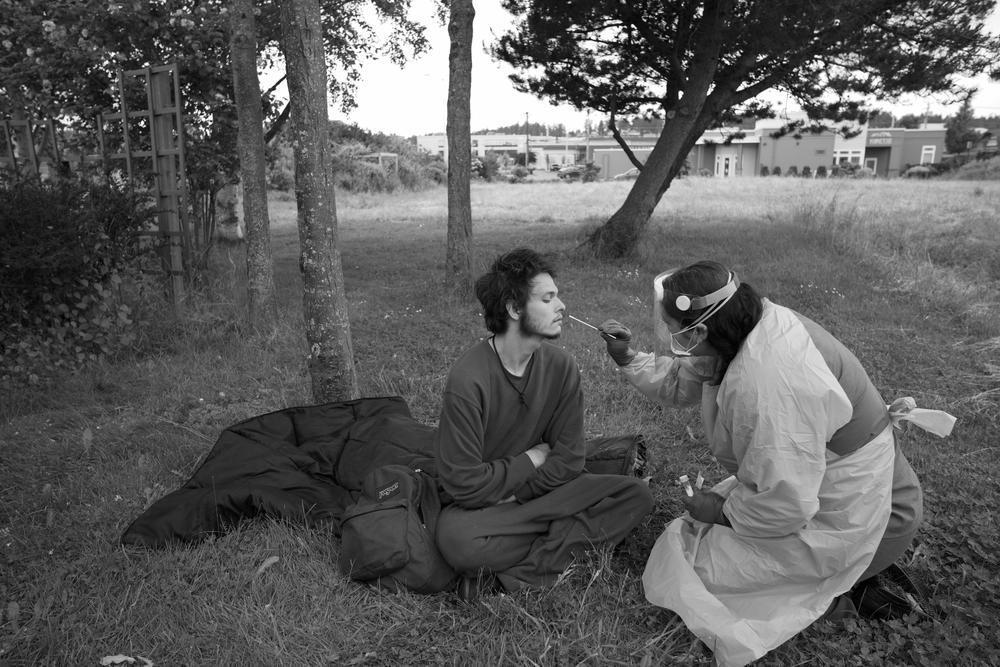
The pandemic gave her clarity of purpose, a moment to put her years of training in epidemiology to use. Masks, tests and vaccines were part of her trade. She knew the island was vulnerable. It had a high concentration of retirees and seniors, and then there were the people living on the margins, some even off grid.
So she got to work, combing the island for anyone who needed her: "There was a job to do and there was an answer: You helped people," says Sierra.
She remembers how the hospital filled up in those early days of the pandemic, when the virus spread through the local nursing home, just a stone's throw away. "We had people who we'd known for a very long time that were coming in, and they were in our ICU," she says. Those who did survive lingered there, even after they recovered, because they simply "had nowhere else to go."
As the adrenaline faded, Sierra started to notice the ripple effects of living with COVID-19, the fraying web of care and connection on the island. "Humans depend on hope. We get through things, because we know on the other side of them it will be okay," she says. "I don't know that I hear a lot of hope from people anymore."
Health clinics had closed. The pool of caregivers for the aging and homebound shrank. And the hospital was struggling to stay afloat. Soon there was talk of cutting the labor and delivery unit — the only one on the island — where Sierra had taken over as nurse manager. If that happened, there would be nowhere for a woman who was pregnant to get hospital care on the island.
Sierra imagined what would happen when things went wrong — how precious minutes would be squandered trying to get off the island to the nearest hospital. She did the math: at least four infants would have died in the past year alone, and "probably more mothers than that, if we had not been here right when they needed us."
For now, labor and delivery remains open. The hospital administrators say they've backed off from the idea, after considering the repercussions. But with money tight, nothing is certain quite yet.
Doug Neal, paramedic
Suddenly, all the calls seemed to just stop. Doug Neal wasn't quite sure what to make of it. He had worked on the island for more than two decades as a paramedic. "The streets were bare," says Neal. "Rarely did we roll out."
The lockdown — and the specter of catching the virus — had kept even some of the sickest people from calling 911 in those early days of the pandemic. Many had medical problems that went untended, sometimes for months or longer. Eventually, Neal would see those patients. And then it would be a true emergency: "Instead of calling earlier, when they know that they're going to need some help, they'd call too late, sometimes."
All that had changed by the second year of the pandemic. Calls started pouring in. In 2021 alone, his emergency medical services crew transported 1,000 more people than ever before. "That's just an astronomical number," he says.
Some of the patients had COVID; others were scared they did and didn't know how else to get an answer. These days, he's spending a lot of time simply looking for a place to bring his patients. Sometimes the hospitals don't have enough nurses on staff, or the right equipment, or enough beds. "You're on the phone trying to figure out where to take someone and everybody's saying, 'No, we're full. We can't take it.'"
Whidbey only has so many ambulances. A journey off the island to the nearest hospital can take at least 30 minutes, if you're running lights with sirens blaring. The more ambulances that leave the island in search of a hospital, the fewer people are left to care for those still there. "It happens, at times, when we're all busy on calls, and there's not another rig available."
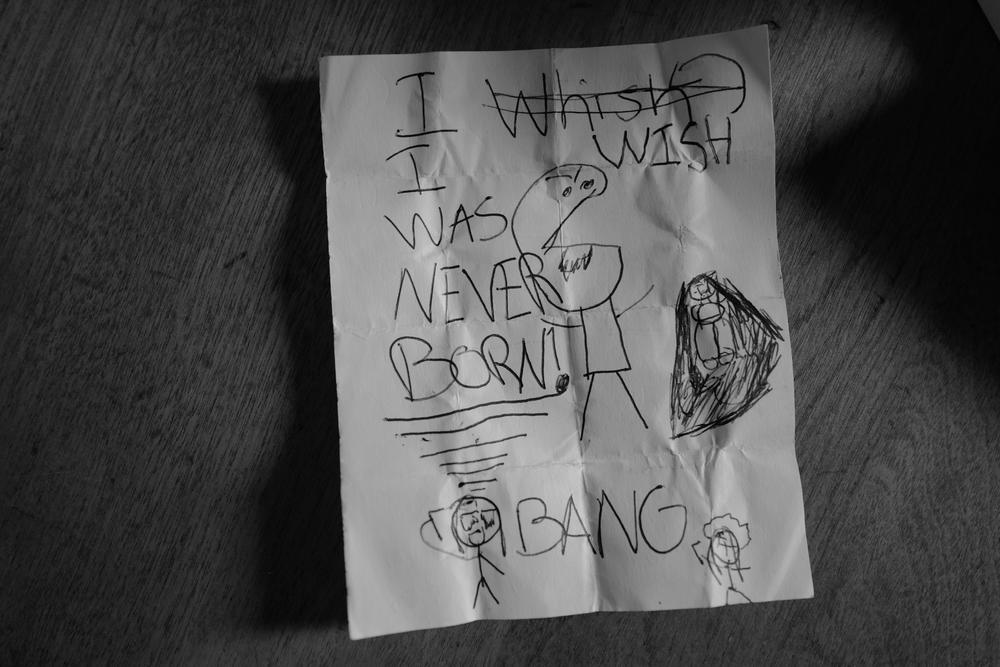
Richard West, therapist and crisis responder
Richard West knows he can't get away from his work — not that he wants to. Maybe, it'll happen at the grocery store or a gas station. "We are in a small community and the chances of us sharing the same space is really high," he says. Invariably, he will run into someone he's dealt with as a therapist and crisis responder. That's the reality of living on Whidbey Island, a place where the need for mental health care eclipses the services actually available. But that's partly why he's there. The small town feel works for him. Sometimes it even reminds West of where he grew up in Oklahoma, as a tribal member of the Muscogee Creek Nation.
Before becoming a therapist, West spent years as a probation and parole officer. When he moved to the island, he saw that sometimes there would be nowhere to send people who needed mental health treatment. If they wanted help, they'd often need to go to Seattle. That meant some people didn't get any help at all. So, he decided to open up his own practice. If people need to see him, maybe because of a court order or a crisis, he tries to see them, even if they can't pay. And when the pandemic came to Whidbey, West didn't go remote. He stayed out there — doing what he does best: connecting with people, talking them down, finding them help. Sometimes he'd tag along with police officers, trying to prop up the fraying safety net in his community.
"I've just seen so much grief and fear and uncertainty," he says. "That just causes some people to kind of unravel at the seams." There's one patient he remembers who'd worked with him for several years. One day, that person killed themself. Others died by overdose. "Those who already had some struggles, it just became magnified," he says.
Even now, West feels the tailwinds of the pandemic in his own practice: "People are just a little more angry and a little more on the edge, and even a little more unforgiving." Family ties are strained or shattered. And the island's capacity to respond is flagging. The mental health infrastructure has withered. Clinics and counselors shut down because of COVID-19. Some have never reopened. West tries to fill in the gaps. "I just try to be a man of my word and offer what we can," he says. "There are so many that aren't getting any help."
Peyton Wischmeier and Chrysalis Kendall, speech therapist, occupational therapist
Peyton Wischmeier has always had a waitlist. There are few other options on the island for families who need a speech therapist, especially if they don't have much money or good health insurance. She doesn't have that problem. WhidbeyHealth Medical Center is a public hospital, so she can take anyone, regardless of what they can pay. That's a good thing, but it leaves Wischmeier with a sense that she can never get to everyone as fast as she'd like, or maybe at all: "It feels like if I am unable to see a child, other opportunities are just really nonexistent."
The pandemic has only underscored how fundamental it is to have this one-on-one time. In a world of masks, visual cues are hard to come by for children who are learning how to move their mouths and make the right sounds. It's no surprise they're seeing an uptick in delayed speech skills, says Chrysalis Kendall, an occupational therapist who works hand-in-hand with Wischmeier. "I call it a sensory hangover," says Kendall, who moved to the island five years ago.
Often the kids who work with Kendall already struggle with how to interpret other people's feelings. The pandemic was profoundly disorienting for them. "Suddenly, all they can see are your eyes," says Kendall, "and that for a kid on the spectrum is the hardest place on your face to look at." And it goes well beyond masks. Kendall still sees the aftershocks of all that social isolation and online learning. "We have these kids who really rely on their external resources for regulation and they're not sure where to go for that," she says.
Lisa Toomey, oncology nurse
Lisa Toomey never downplayed the coronavirus, even when it was just a seemingly distant news story from overseas. It wasn't her first pandemic. About 40 years ago, Toomey confronted the HIV/AIDS crisis at the start of her nursing career. She still remembers the fear, how even some doctors and nurses wouldn't touch their own patients. With this new virus, Toomey wasn't going to take any chances with those under her care. Their immune systems were too fragile, suppressed from cancer treatments. She says that's why her oncology unit, "the MAC" for short, locked down before the rest of the hospital.
Soon, it was virtually unrecognizable. They'd always taken extra care to keep their patients safe. Nurses would wear gloves and chemo gowns, but COVID-19 ushered in an entirely new way of doing cancer care. No more hugging and holding hands. Family members were prohibited. The laughter and smiles seemed to fade. "We just felt like we jumped over a cliff and we were cut off from each other," she says. "The lifeline was our masks and our gloves, that was our lifeline to continue to hold onto one another." Being on Whidbey meant they knew most of their patients, these were their neighbors and friends. "We got very, very protective, and that's why no one got sick," she says.
In those early days, Toomey says the oncology nurses made a pact: to keep their patients safe, they would have to live like them. No traveling. They hit the brakes on their social lives. Even Toomey's own family was kept at a distance initially: "I'd come home and I didn't hug my kids and my wife for months."
At work, the nurses would take care not to fall back into old habits. They'd eat lunch in their cars by themselves. Toomey had spent years teaching younger nurses how to do the job. Now she found herself learning again. She discovered how to offer that same comfort to her patients, using only her eyes and tone of voice. And when vaccines arrived, she took on yet another role: the "scheduling queen." She booked countless vaccine appointments for her patients.
Now, at long last, they're finally back to hugging. Family members have just started to trickle in again. Toomey wouldn't call it a return to normal. That probably will never happen. "And that's okay," she says. "We talk about how fragile life is, and how it can change so fast, and how we really appreciate what we have – being able to wake up every day, being able to gather together. That appreciation, that will never be forgotten."
If you or someone you know may be considering suicide, contact the National Suicide Prevention Lifeline at 1-800-273-8255 (En Español: 1-888-628-9454; Deaf and Hard of Hearing: 1-800-799-4889) or the Crisis Text Line by texting HOME to 741741.
Copyright 2022 NPR. To see more, visit https://www.npr.org.