Section Branding
Header Content
Health care has a massive carbon footprint. These doctors are trying to change that
Primary Content
Inside an operating room at Magee Women's Hospital in Pittsburgh, Noe Woods stands in her blue scrubs next to a black operating table.
Woods, an Ob-Gyn, knows this room well.
"I've operated in this room many times over the last 14 years. I've probably taken out uteruses, polyps, ovaries, ectopic pregnancies," Woods said.
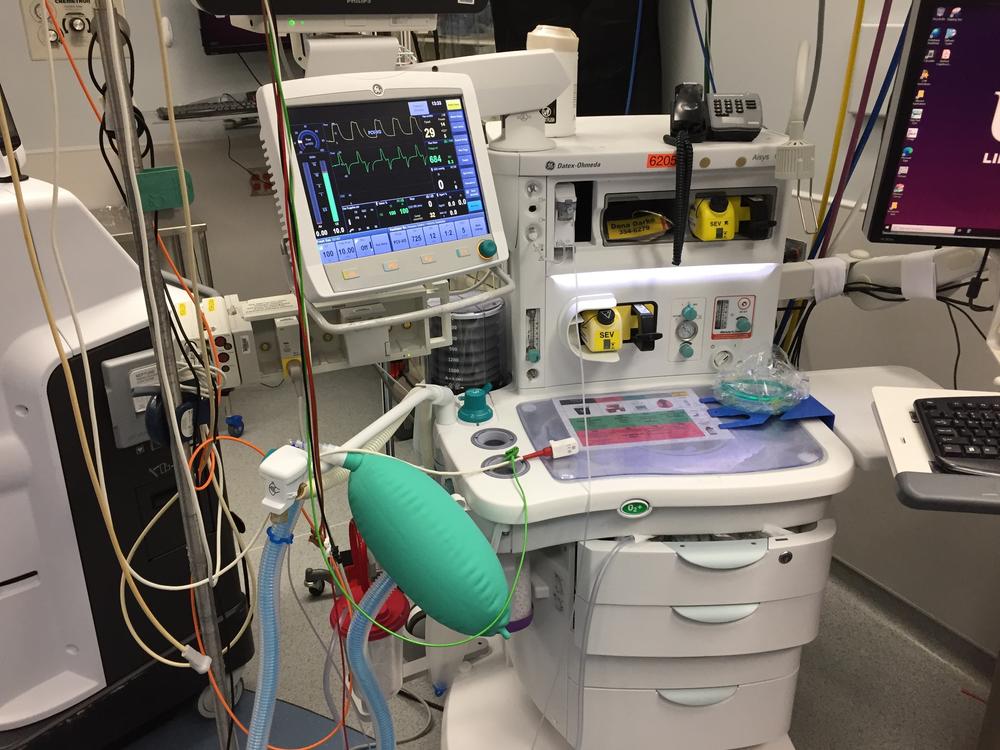
Operating rooms are central to what hospitals do, but they're also at the root of a problem Woods and others at the University of Pittsburgh Medical Center (UPMC) are trying to solve: how to reduce carbon pollution.
"Operating rooms are a pretty small part of the physical footprint of a hospital, but they produce an outsized amount of the waste," Woods said.
Hospitals are some of the biggest carbon polluters almost no one thinks about. The American health care system accounts for an estimated 8.5% of the country's carbon footprint. This sector emits climate warming pollution through a variety of sources including energy used to run facilities, transportation, products and what gets disposed of.
I've known Woods for 20 years, but only recently found out about her climate work at UPMC, western Pennsylvania's largest hospital system.
Woods struggled for years to get her colleagues to focus on human-driven climate change. "In the beginning it was just so slow, it was so weird and alternative," she said. "A lot of people gave me a pat on the back like, 'Oh, I'm so glad you're doing that.' "
Woods eventually burned out. But two years ago she found a handful of other doctors at UPMC also interested in climate change. They formed Clinicians for Climate Action, which quickly grew to over 500 doctors, nurses and others inside UPMC's 40-hospital system.
"Everyone now, because the world is on fire, everybody's sort of looking at each other saying, OK, now we really do have to do something," Woods said.
The group's members recently got UPMC to phase out desflurane, an anesthetic gas that's 3,700 times more potent than carbon dioxide. They've also reduced cafeteria food waste and cut down on single-use items.
For example, UPMC Children's Hospital of Pittsburgh switched to reusable fingertip sensors to measure blood oxygen levels. That idea came from Isabela Angelelli, a pediatrician at Children's Hospital and a co-chair of the climate group.
"Children's Hospital goes through 180,000 of them a year. That's $1 million that goes in the trash," she said. In the months since switching to reusable sensors, they've decreased their consumption of sensors by 63%, Angelelli said. "We're saving in the thousands every month."
Angelelli said it's been easy to get hospital staff to buy into the idea of reducing waste. "It comes all from people at the bedside coming to us and saying, 'My heart hurts when I throw all these things in the trash,'" Angelelli said. "The nurses would come and tell me, 'Count me in, I'm totally in.' Everyone wants to be part of this."
Around the country, health care workers continue to grapple with their industry's massive carbon footprint.
Jodi Sherman, associate professor of anesthesiology and epidemiology at Yale School of Medicine, said unnecessary procedures are a part of the problem. She said they improve hospitals' bottom lines but not patient health.
Sherman said hospitals have also gone overboard on using disposable items to meet mandates to prevent infections.
"We're at a point where we're throwing away complex robotic surgical instruments," Sherman said.
High-end scalpels get trashed, but also blood pressure cuffs, bed linens, pillows and patient gowns. Each requires energy to make, package and ship, most of which still comes from fossil fuels — the main cause of global warming.
"These are all becoming single-use disposable," Sherman said. "We're dripping in waste."
An influential national hospital accrediting body, the Joint Commission, backed down from a proposal to mandate facilities count their emissions after hospitals complained. For the time being, the commission will offer a voluntary certification in sustainable health care.
Sherman thinks a national mandate to lower emissions is the only way to solve U.S. health care's outsized carbon footprint. For now, however, there are only voluntary measures like the ones at UPMC.
UPMC signed a White House pledge to halve carbon emissions by 2030 after Noe Woods and her colleagues collected more than 200 signatures for a letter urging climate action.
"We didn't advertise it. We just emailed it to people who we thought would," Woods said. "And you know, within a week and a half we had enough signatures to send it."
The group also asked UPMC to establish a sustainability office to measure and then reduce its greenhouse gas footprint. Woods said she was surprised when UPMC agreed and then actually created the Center for Sustainability.
"It [the center] has names on the doors. It has employees," Woods said. "They are calculating things. It's unbelievable."
The office's latest hire is an energy engineer who will help figure out how to lower UPMC's energy use and source more of it from renewables.
Woods said the momentum to push for climate action has gained quickly among her peers.
"You don't find doctors very often volunteering their time for a cause consistently, persistently, meeting after meeting. Showing up with new ideas, and then another person who's interested (comes) and then another," Woods said. "Everybody cares."
Copyright 2023 The Allegheny Front. To see more, visit The Allegheny Front.