Section Branding
Header Content
When poor Black communities were struggling with COVID, this surgeon stepped in
Primary Content
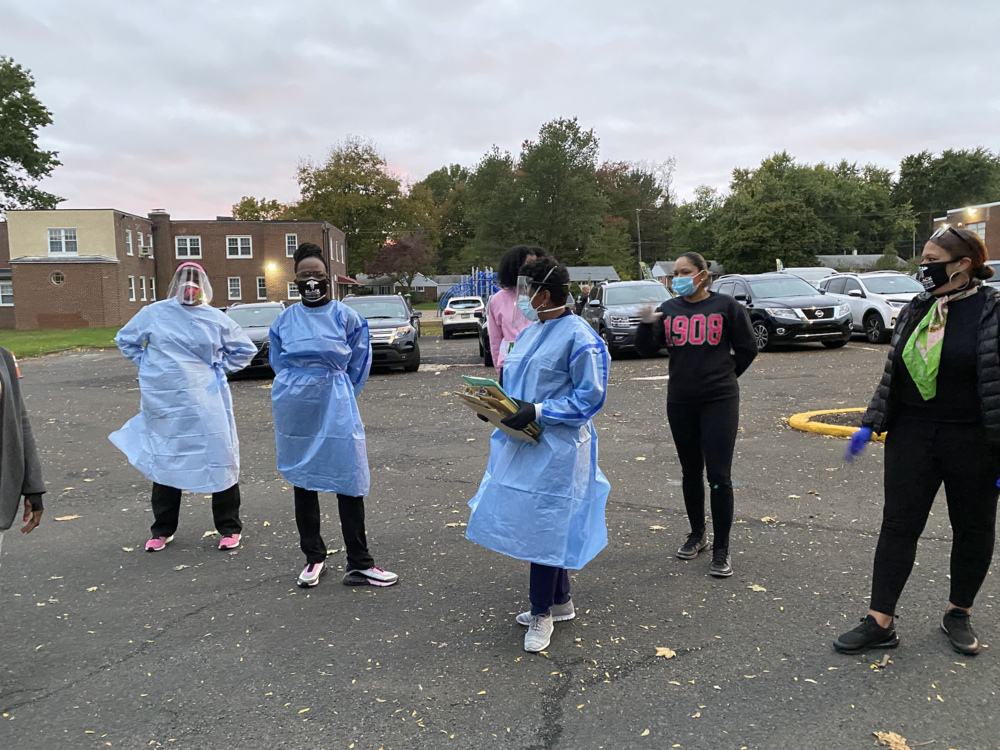
As a pediatric surgeon, Dr. Ala Stanford operated on children, infants and sometimes fragile premature babies. But when the pandemic hit in 2020, she left her job to found the Black Doctors COVID-19 Consortium, setting up shop in parking lots, churches and mosques where she provided tests and vaccines to underserved Philadelphia communities like the one she grew up in.
"I believe you go to the most vulnerable," Stanford says of her outreach. "I've saved more lives in a parking lot than I ever did in an operating room."
Early in the pandemic, Stanford realized that bureaucratic red tape was preventing vulnerable community members from getting access to COVID testing. She responded by contacting LabCorp, and ordering that the tests be billed directly to her.
"I wanted [testing] to be barrier free," Stanford says. "I just said, 'If you have been exposed and you need a COVID test, come to us.' That's it."
After vaccines became widely available and COVID-19 became less deadly, the consortium expanded its services by establishing clinics in Black communities around the city. Stanford writes about her experiences with COVID and in community health in the new memoir, Take Care of Them Like My Own: Faith, Fortitude, and a Surgeon’s Fight for Health Justice.
The title of her book borrows from a guiding principle of her medical practice: "With every child I operate on, with every adult that I cared for during COVID and beyond, ... I just try to treat them like I would pray someone would treat my children and my husband," she says.
Interview highlights
On setting up COVID-19 testing sites for underserved communities
All of the data where people were having higher incidence of disease, the demographics, it was all on phila.gov. … Once I had those zip codes, I put them in order of sickest to least sick. And then I said, "OK, it's Black people in the city of Philadelphia that are three times more likely to contract the disease and die." So where do they trust? And for me, in my experience, it's mosques. It's churches, it's community centers. And so I asked my pastor to help me identify a church or a mosque in each zip code where ... the disease was the highest and that's where we targeted. We went to where the need was the greatest. And we set up shop right there.
On how the 2020 pandemic “shelter in place” protocols impacted poor communities
When you're saying to everyone, “Shelter in place,” and “Don't go out into the public,” but you can't afford to shelter in place because you have to go out into the public to support your family, when you're saying, "Buy a bunch of food for a month and keep it stored,” and people don't have the money to do that — it's sort of like the adage of telling a bootless man to pull himself up from his own bootstraps. It's like the recommendations were applicable for certain socioeconomic tiers in society and not for others. And so, in my mind, I hope we never have another pandemic again or a public health crisis. But those who have the greatest need are where you put the emphasis. And it's not to say that you can't take care of everybody at the same time, but there should be more emphasis on where you will see the greatest death and disease.
On the narrative that Black people wouldn’t get the COVID vaccine because of distrust in the government
Being [a] physician scientist, I said, "Why don't we ask them?" So it was October of 2020 and it was flu season. And so in addition to doing COVID tests, we were also doing flu shots. And ... when they came in, we did a survey … and we asked them if a vaccine were available today, what would make you take it? What would you be concerned about? … What I learned more than anything is that the majority of people said that they did trust the government to produce a vaccine, and yes, they would take it.
On why she got the COVID vaccine on camera
So when the vaccine came about, people had already started to develop a level of trust with us. But even that wasn't enough for everyone. And so we led by example and we, on camera, went to get vaccinated. A lot of folks from the Black Doctors Consortium live on camera, we were vaccinated. And because people were saying, “Doc, when you say it's OK, I'll get it. When you roll up your sleeve, I will get it.” …
We listened to what people's fears were and … some of it was, “I'm scared of needles.” … Or someone said, well, “I'm allergic to eggs, so I think I might be allergic to the vaccine.” You had to ask rather than assume you knew 1.), that they didn't want it, and 2.), the reason why. And so I let the people educate me so that I knew best how to care for them.
On middle- and upper-class people trying to get vaccines that were specifically for underserved communities
When I started seeing Teslas and Range Rovers in the parking lot in North Philly, I was like, “What is going on here?” Because most people take public transportation anyway. And these were some very expensive cars in my parking lot. And I would say it doesn't help if you come to this community and take a vaccine and go back to your place in the suburbs or wherever, where you're sheltering in place in your own bubble, and you're not interfacing with the public, and then the people who are interfacing with the public -- they're going to work and they're more exposed and they're more likely to contract the disease -- don't have it. It doesn't make the pandemic end any sooner if you do that. It's not going to allow you to go on vacation any sooner if you take from those who are the ones who are most at risk. …
And what we started to do was oversample from the zip codes where the positivity rate was the highest, and people told me I was discriminating. Who was I? I didn't have the right to do that. And I said, “This is a public health crisis and in a public health crisis you go to those who have the greatest disease, the greatest morbidity, mortality, and death, that's where we went, right?” And later the city did the same thing. But for me, I got lots of sort of hate texts and direct messages and all those sorts of things, but I knew it was the right thing to do, so I just pressed on.
On the American Medical Association classifying racism as a public health issue in 2020
You have to acknowledge that bias exists in health care. So it's great that the American Medical Association says it exists. But do you believe it? As someone in health care, do you believe that you play a role because of your own lived experience and bias that you bring into the exam room and into the operating room? And I think until the caregivers and educators acknowledge that we all have that bias, that we believe that we do, that we identify ways that we can change it and that we act on those things we identify, and then we share it with others. ... Until we do that, that's when you see real change.
Sam Briger and Thea Chaloner produced and edited this interview for broadcast. Bridget Bentz, Molly Seavy-Nesper and Meghan Sullivan adapted it for the web.