Section Branding
Header Content
Mental Health And Police Violence: How Crisis Intervention Teams Are Failing
Primary Content
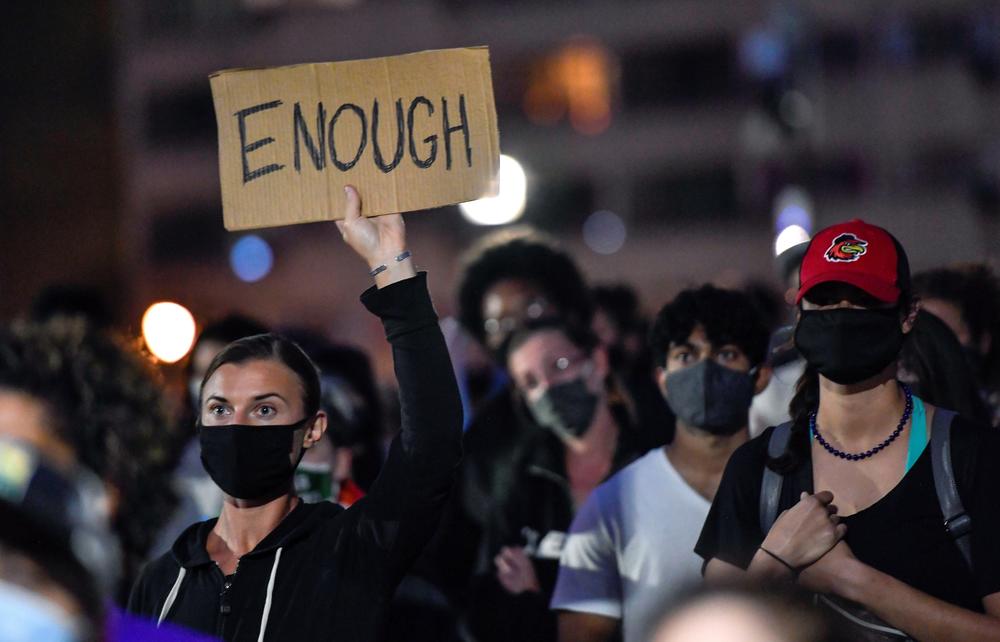
Nationwide protests over police accountability and racial justice have reenergized longstanding efforts to fundamentally change how police departments respond to someone in a mental health emergency. Many are calling for removing or dramatically reducing law enforcement's role in responding to those crisis calls unless absolutely necessary.
Since 2015, nearly a quarter of all people killed by police officers in America have had a known mental illness. Injuries, too, are common although they are less carefully tracked. There's anecdotal evidence that botched encounters between police and people in a mental crisis are up during the pandemic.
One of the many examples: the recent shooting of a distraught 13-year-old boy with an autism spectrum disorder by Salt Lake City police after his mother called officers to report that her son was having "a mental breakdown." The teenager is recovering from serious wounds. Then there's the recent police shooting of a homeless man in crisis in Buffalo, N.Y.
Still, many departments appear reluctant to abandon a widely-used program for handling mental health and substance abuse crisis calls, called crisis intervention teams or CITs, even though the programs have proved largely ineffective. Even some proponents and trainers of CITs now say the model has been misread and poorly implemented by many departments.
Vivid example of the shortcomings of CITs
Rochester had created one of New York state's first crisis intervention teams. And the March asphyxiation death of Daniel Prude there during a police confrontation, which has badly shaken the city and its police and political structure, offers a vivid example of the shortcomings and misreading of CITs.
Around 3 a.m. on March 23, Daniel Prude was unraveling. A light snow was falling when police confronted him. The 41-year-old Black man was wandering the street, naked and babbling. He was suffering a mental breakdown exacerbated by drug abuse.
Officers handcuffed Prude and put a hood over his head, apparently to stop him from spitting at them. It was the early weeks of the coronavirus pandemic in the state. Three officers pinned Prude to the ground as he became increasingly agitated. They pressed his face into the pavement for two minutes, one officer pushing heavily on Prude's head, according to bodycam video of the encounter. Prude stopped breathing. He was taken off life support at a local hospital a week later.
"I placed the phone call for my brother to get help, not for my brother to get lynched," said Joseph Prude, who told police that his brother, Daniel, was having a mental breakdown and was on drugs.
Daniel, who had recently arrived at his brother's from Chicago, had already been seen by a local hospital for erratic behavior and suicidal thoughts the previous day.
A lawsuit by the Prude family says Prude was undergoing an "acute manic, psychotic episode." The Monroe County medical examiner ruled his death a homicide, citing asphyxia due to physical restraint by police and acute intoxication from the drug PCP as causes of death.
"We know what happened that night for Mr. Daniel Prude, and we don't want to see any more names," says Krystal Schulik a drug and alcohol counselor in Rochester.
No to handcuffs, hoods. Yes to calm talk, deescalation
Schulik and many others in the mental health field in the city are trying to change how the police respond to these kinds of crisis calls. No to handcuffs and hoods. Yes to calm talk and careful deescalation.
"Change your tone of voice, your body language, hell, you might have to get on the ground with him! Give him eye contact. All of that is so important when deescalating such a scale of an event," she says of the Prude case. "He was not well."
Some Rochester police, in theory, were trained to do just that – to recognize and deescalate confrontations with someone in a mental health meltdown; someone just like Daniel Prude. Rochester created its Crisis Intervention Team in 2004 after a case similar to Prude's.
These teams and their trainings grew out of Memphis, Tenn., in 1987 after police fatally shot Joseph DeWayne Robinson, 27-year-old who was in a mental crisis and cutting himself with a butcher knife.
CIT programs and trainings soon spread from Memphis to thousands of departments across the country. Yet despite the proliferation and popularity of what came to be called the "Memphis Model" some key people who advocate for the program say it has often been misapplied and misconstrued by law enforcement.
'They're not doing anything about what a CIT really is'
" 'All we have to do is give them little training, and send them out there to handle crisis situations.' That's the kind of mentality, the thought process, that we have utilized for way, way too long," says Ron Bruno, who had a 25-year career as a police officer and is now executive director of Crisis Intervention Team International. The group runs trainings and works to change the dynamic between law enforcement and people in a mental health crisis.
Bruno says a handful of departments have done it right. But others, too often, see CIT training as merely as a check-the-box, 40-hour exercise. "They're not doing anything about what a CIT really is," he says.
The biggest breakdown, Bruno and others say, is that cities and counties too often fail to carefully integrate the program into the wider behavioral mental health care system and route calls away from police. "If you keep throwing money at training officers, and that's all you do, and not address the system around mental health care, you'll continue to have nothing but problems."
To critics, the way these crisis teams have been built and proliferated is yet another example of police tinkering with reforms that look nice for police chiefs and mayors but fail actually to make substantive change.
A non-law-enforcement crisis response team
Woefully inadequate mental health services across the country means police are usually the first to respond to someone in a mental health and/or substance abuse crisis. It's estimated that those situations make up at least 20% of police calls for service When done right, advocates say, mental health crisis teams remove police from responding, unless absolutely necessary.
"We need to build community resources that can respond and take care of a crisis without having law enforcement involved," Bruno says. "If we build the crisis response system, that is non-law enforcement, we will get more people connecting before it hits that level of danger."
He says the moment is now ripe for more cities to create specially trained, mobile crisis response teams made up of mental health clinicians, medical professionals and, perhaps, peer support specialists who've been through mental health or drug and alcohol challenges. People who can lend an empathetic ear, deescalate, and help channel the person to services, not jail.
"All I'm talking about is a non-law enforcement crisis response team. Whatever disciplines you want to make up that team, it works," Bruno says.
But that's rarely happening.
Only a very few cities have created that kind of system. But there is a pioneering program in Eugene, Ore. There, a three-decade-old program named Crisis Assistance Helping Out On The Streets or CAHOOTS created by White Bird Clinic runs mobile crisis intervention response teams that are tied directly to the area's 911 system.
Timothy Black, White Bird's consulting director, is leading efforts to help other communities replicate the CAHOOTS-style program. One of the biggest obstacles in scaling this kind of program, Black says, is overcoming the widely held perception that people in a mental health crisis are inherently dangerous. "It's our experience that folks in crisis just aren't dangerous," Black tells NPR.
"If we can shift away from really applying morality to these situations we start to recognize that, you know, these crises of all emerge because a need has gone unmet. And the response is really about meeting people where they're at and identifying those needs and supporting somebody."
Experience there shows the responses, except in very rare cases of violence, he says, are best handled by clinicians and medical professionals. "It's really, really a misnomer to say that the only response [to] people in crisis can be a response that involves the tools of force, like a badge, a gun, and handcuffs."
No replacement for adequate mental health care system
Still, police crisis intervention teams remain the dominant model. They've been around for more than 30 years and have spread to more than 2,700 departments.
Yet few of them carefully track the program's outcomes or have clear benchmarks to measure success.
"One of the things that has been missing from the conversation until quite recently is that it's still no replacement for an adequate mental health care system in a community," says professor Christy Lopez who directs the Innovative Policing Program at Georgetown Law.
She says these police crisis teams have proved useful and important, but only to a point. "It's often using police officers to address a problem when they're not needed and might even make things worse. I wouldn't say it's window dressing, but I think it can be problematic if it makes us think that's all we need to do," Lopez says.
A study last year in the Journal of the American Academy of Psychiatry and the Law concluded that police crisis intervention teams have only modestly helped reduce arrests of people with a mental illness and kept them out of the criminal justice system.
"The (CIT) programs have been effective in that way, that there are more people who are brought to psychiatric emergency rooms or to behavioral health clinics than down to the Hall of Justice," says Dr. Reneé Binder, who directs the Psychiatry and Law Program at the University of California, San Francisco, and was one the authors of the crisis team study. "Because people who have psychiatric issues don't belong in jail and practically everybody agrees with that."
But Binder says the study also concluded that CITs have failed in a fundamental goal: to deescalate and reduce violence to citizens and police alike. "It hasn't shown any consistent reduction in the risk of mortality or death during emergency police interactions," she says. "So it has not significantly decreased the number of individuals who are killed or injured."
Rochester Mayor Lovely Warren has apologized for what she called multiple, systemic failures that led to Prude's death, including longstanding racial inequities in the city. "Daniel Prude was failed by our police department, our mental health care system, our society. And he was failed by me," Warren told a press conference. Warren, who is African American, called for facing racism head on and vowed to do more herself.
"We cannot continue to fail Black lives this way. We can't improve our city or improve our nation until we face the reality, the undeniable truth: Racism is alive and well in every system in America. And the buck stops here today with me at City Hall," Warren said.
Rochester police would not respond to detailed questions about its crisis intervention team or whether any of the officers in the Daniel Prude case had any of that training.
Last fall, five months before Prude's death, Sgt. Steve Boily, who was then the commander of Rochester's CIT, said in an interview with local TV station WHAM that the program was effective and working well.
But Boily also conceded that additional crisis training was unlikely to be enough. "Some people are too ill, too angry, too violent that no matter what training, some bad things are gonna happen," he told the station.
"Some bad things are gonna happen" now echoes eerily prescient in Rochester where the police chief has been fired, street protests continue and Prude's family is demanding answers, changes and justice.
Copyright 2020 NPR. To see more, visit https://www.npr.org.