Section Branding
Header Content
In Atlanta, A Wave Of Coronavirus Deaths And The Questions Left In Its Wake
Primary Content
On the evening of Feb. 20 at an assisted living facility just on the edge of southwest Atlanta, Ernestine Mann stood in front of her peers to read aloud a proclamation commemorating Black History Month. She was dressed for the occasion: delicate earrings and a flowy blouse with a little hint of shimmer.
"Good evening everyone," Mann said as her daughter Karla McKinney filmed. "This is my first year living here, and I'm having a great time."
Mann moved into this facility, Arbor Terrace at Cascade, in August 2019 and quickly became a prominent community member. She was a leader in a group tasked with welcoming newcomers; once, she'd greeted a woman who was deaf by seamlessly switching to American Sign Language, a skill she'd learned years earlier.
"She was not over there wasting away," McKinney said. "She wasn't the resident that just kind of showed up for the dining hall and then just stayed in her room. She had a really nice social life."
That particular night in February, Mann was standing before her new neighbors, reading a document celebrating "the remarkable accomplishments and lasting impact of our country's great African American leaders and citizens."
It was fitting she would read this particular proclamation to this particular group. Many of the residents fit that description. There was Bernice Foster, known for her musical talent; Dr. Delutha King, co-founder of the Sickle Cell Foundation of Georgia, and his wife, Lois King; Blanche and Eddie Johnson Jr., married for 63 years; Edgar Lewis, a retired Air Force lieutenant colonel; and, of course, Mann herself, a teacher for three decades.
In a little more than two months, all of them would die from COVID-19.
In all, at least 17 residents died, 54 residents tested positive, and 36 staff tested positive. It is the worst outbreak among the 11 Georgia locations managed by the Arbor Co. There's another key difference between this Arbor Terrace and the others: In Georgia, it is the company's only facility in a predominantly Black neighborhood. That has left the families of the dead to wonder what exactly went wrong and whether racism played a role.
NPR looked into what happened at Arbor Terrace at Cascade to try to answer that question. Through government records and interviews with families, residents, and former staff, a more complete picture of the outbreak emerged. The Arbor Co. left Cascade residents and staff inadequately protected at a crucial moment, and this particular facility could not afford missteps. Systemic factors — including its location in Atlanta and its particularly vulnerable population — made this place both more susceptible and more vulnerable to the virus and, perhaps, its staff less equipped to respond.
The result reflects a grim national pattern that has endured throughout the pandemic's many months: Black Americans are getting and dying from COVID-19 at higher rates than white Americans. The outbreak at Arbor Terrace at Cascade offers a glimpse into factors that contribute to that disparity at a place where some of the families did not expect it to play out.
"Even though you achieved all these things, at the end of your life, you are in essence, and I hate to say this, you were in some COVID-infested center," said Tricia Johnson, the daughter of a resident who tested positive but survived. "I mean, their brand has definitely been tarnished, but it doesn't appear it's going to be tarnished in the white areas."
"The crème de la crème"
Arbor Terrace at Cascade is just off Cascade Road, a major thoroughfare in southwest Atlanta. A tall grove of trees shields the building from the main road, making it feel apart from the bustle of the nearby Home Depot and Walmart. Its colonial revival facade is homey: red brick and pale yellow siding with slate-colored shutters.
The area around the facility is simply known as Cascade, and the neighborhood has had its share of notable residents over the years: former Atlanta mayors, baseball legend Hank Aaron and John Lewis, the late civil rights leader and congressman. But until the mid-1960s, much of the area was white.
"It was one of those white flight things where the Blacks were moving into the area more and more," said the Rev. Gary Dean, senior pastor at Hoosier Memorial United Methodist Church, located near Cascade Road. "Of course the whites, they left, and the community became basically all Black."
After Arbor Terrace at Cascade opened in 1999, it came to mirror its surroundings. The Black movers and shakers of Atlanta moved in. Talk to people who have worked there, and they'll tell you stories of doctors, lawyers, teachers, city planners, a Tuskegee Airman. Marcus Davis, a former maintenance director at the facility, said living in the Cascade area was a "badge of honor" and that Arbor Terrace at Cascade, where it was common to pay more than $4,000 per month for an apartment, became a "status symbol."
"It was like being at grandma and grandpa's house every day. You had some of the most intelligent, sweet, kind, loving people," Davis said. "A lot of the people who resided at Arbor Terrace at Cascade were intricate parts of Black history throughout Atlanta and throughout the United States."
When the National Center for Civil and Human Rights opened in Atlanta in 2014, Davis said they took a group from the facility to the museum. He listened to the residents swap stories from the civil rights movement.
"They were firsthand accounts," he said. "Oh my God, it was unbelievable."
When Mann's family was searching for a facility, her daughter Karla McKinney said they landed on Arbor Terrace in part because it was near where her mother had lived, and because she already had friends there.
"It was looked upon as one of the crème de la crème of assisted living facilities," McKinney said.
''If I knew what I know now, I could have just lost my job"
In the weeks leading up to the first highly publicized outbreaks in the U.S., Jazmine Heggins, a former resident assistant who worked at the facility at the time, remembers feeling like some employees weren't as worried as they should have been.
"It kind of was like, 'Oh, that's not going to make it to the United States. We're not going to have anything to worry about.' It was kind of just like something that was made up almost," she said.
But then, Heggins said, staff and residents started to get sick with something. And by late March, she did, too.
She woke up exhausted on a Friday morning. By Sunday, she had aches and a sore throat. She later wrote on her blog that "it was as if someone had beaten me with a baseball bat overnight."
Heggins told NPR that she reached out to work, saying she thought she had caught something from the residents. The staff member who replied said she couldn't call in sick and should tough it out.
Heggins said she felt confused: The company had explicitly told them not to come into work if they felt sick. That was in line with Centers for Disease Control and Prevention guidance. But now she was being told to come in.
"It was like they were telling us one thing, but then they really meant, like, it doesn't actually matter. We just have to tell you this," Heggins told NPR. A few hours after she got to work, she said she developed a fever. At that point, she said, she was allowed to go home.
While Heggins was out, she said she started getting phone calls from coworkers, telling her about the residents who died.
"It was like someone calling you and telling you, 'Hey, your grandma just passed away, and you may have given them COVID and they just passed away,' but it was over and over again," Heggins said. "Everybody that you take care of every day, say good night to and tuck in to sleep and wake them up in the morning, they're dead now."
She said she eventually asked them to stop calling.
"I was going to sleep crying every night. It was just too much," she said. "I was potentially going to lose my job, but if I knew what I know now, I could have just lost my job."
Another former staff member, who asked not to be named, said other coworkers also felt pressured to come to work and that leadership at the facility told them they couldn't go home if they didn't have a fever, even if they were showing other symptoms.
"Just as simple as that," the staff member said. "Most likely you're getting fired."
That person also remembers working while symptomatic. One day sticks out in particular, when six or seven residents fell ill at the same time.
"They were throwing up. They were extremely weak. They were having diarrhea. People were clammy and we're trying to get them going to the hospital," the staff member said. "I just remember sitting down telling my other coworker, 'I can't make it through the day.' I said, 'Something's wrong with me and I'm not feeling well.' My whole body was aching and it's all of my strength just to make it through that day."
In a statement to NPR, Judd Harper, president of the Arbor Co., said: "Before the pandemic, Arbor Terrace at Cascade had policies, practices, and procedures, which instructed staff not to come to work with illnesses or physical conditions that may pose a risk to their or others' health and safety. During the pandemic, we re-emphasized that policy and reminded staff of the policy in daily huddles starting on March 3, 2020."
According to Harper, Arbor Terrace at Cascade also took the staff's temperature and had them change clothes when coming to work, and tracked the symptoms of staff who were sick. Harper also told NPR the company paid for coronavirus testing for staff, increased their paid time off, provided hourly bonuses to healthy employees, and provided financial assistance for child care, among other initiatives.
''She didn't have to go this way''
March 25 was the last day McKinney and Bill Mann saw their mother alive. Arbor Terrace at Cascade began restricting visitors on March 12, but by the end of the month, they were allowing window visits. The family came wearing masks and gloves.
"As we were watching and waiting for my mom to come to the window, we could see her coming across the lobby and she was toddling like a baby just beginning to walk," McKinney said. The family knew then that something was off, McKinney said, but tried to stay cheerful.
"She was able to talk but, see, if you knew her, [when] my mom spoke, she spoke strong," Bill Mann said. "This particular time she sounded extremely weak. It was almost to a whisper, and that's just not like her."
Their mom seemed dazed. Her eyes were darting around as if she just couldn't fix her gaze on anyone. She had trouble recognizing her granddaughter.
"We ended up not staying as long as we thought we might have because she clearly was tired and something wasn't right," McKinney said. "When we did get ready to go, she stood up and she stumbled."
McKinney called the facility afterward to have someone check on her mom. And the staff agreed that something was wrong. Mann had been having bouts of diarrhea. They called an ambulance. Marian Hatch, one of Mann's closest friends at the facility, watched as her friend was taken away.
"I saw her. I think I knew she was sick," Hatch, who is 92 and tested positive but survived, told NPR. "The very last time that I saw Ernestine, when she was on the gurney, when she was in the hall waiting to be carried away, I didn't go over to her. I waved at her."
At Piedmont Atlanta Hospital, Mann was first diagnosed with pneumonia.
"Once she got to the hospital, you know, we're blowing up the hospital [with calls] trying to find out what is going on," Bill Mann said.
Her coronavirus test came back positive on March 27. She was placed on oxygen. On March 28, she seemed to be doing better. But by the next day, she had taken a turn for the worst. That morning, a doctor called, saying Mann was agitated and pulling at her oxygen mask. The hospital staff wanted to see if the family could calm her down over the phone.
"I still try very hard to get the sound of her voice out of my mind, even to this day. She said, 'Come help me, help me, help me, you all, please come help me,' " McKinney remembered. The family couldn't visit, because of COVID-19 restrictions.
"To hear her crying out for help, to know that I couldn't get there, it's just been very emotional for me to have that memory of her," McKinney said. "And now, learning more about COVID victims, they seem to feel like they're drowning. That's what I'm told. And just having that thought that my mom was in that predicament, it's just really hard."
Bill Mann remembers praying with his mom. Afterward, he said she seemed more at peace. "After the prayer she said, 'Thank you so much, I really needed that,' " he recalled.
A doctor called again later that day, asking about end-of-life decisions, and whether or not they would want to resuscitate.
"I just didn't see it coming," McKinney said. "I just didn't understand why those kinds of questions were being asked."
Later on, another call: Their mom had stopped breathing on her own.
"The doctor described what it would be like to be on a ventilator, and it was pretty much to prolong the inevitable, and she would suffer," McKinney remembers. "We had to make that heartbreaking decision to let her go."
Ernestine Mann died in the afternoon on March 29. She was 84.
"I understand we are all on the clock and sooner or later we have to go, but not like that," Bill Mann said. "She didn't have to go this way."
Ernestine Mann's death was at the start of a wave of others at the facility. Nancy Finney died the next day. On April 3, Dr. Delutha King and Bernice Foster both died. King had been sent back and forth between different hospitals and the facility at least twice before he died, according to his son Ron Loving.
Hattie Jay died April 5. She had tested negative for the virus, but her daughter Perdita Fisher believes she died because of the stress of isolation. Eddie Johnson Jr. died April 5 and his wife, Blanche, three days later. A photograph of them holding hands at the hospital went viral.
Catherine Hendrix died April 6. Her son Cedric said he still sometimes drives by the facility, wondering what went wrong. Four day later, Lois King, Delutha's wife, died on the day her husband was buried. Dorothy McGirt and Gloria Bolds both died April 12. JoeAnn Snead had only lived at the facility for a little more than two weeks before she was sent to the hospital, where she spent about a month before she died on April 21. A week and a half after that, on May 2, Edgar Lewis died.
At least 17 were dead of COVID-19 by the end, though state records differ on whether the final death toll was 17 or 19. NPR was able to confirm the names of these 13 through family interviews, news reports and obituaries. And somewhere among all those deaths, there were at least four others whose names we couldn't find at all.
"We weren't just going to leave them by themselves"
Four families, including Mann's, have ongoing lawsuits against the Arbor Co. The lawsuits allege that staff failed to wear personal protective equipment, or PPE; that asymptomatic staff who had been exposed to COVID-19 continued to work; and that the company failed to restrict outside visitors. The company denies any wrongdoing.
In April and May, the Georgia Department of Community Health investigated complaints related to the outbreak at Arbor Terrace at Cascade and did not find any rule violations.
The company declined NPR's multiple requests for an interview, but it sent a statement from Harper, the company president, which is referenced throughout this article, and also answered questions in writing.
"Like the rest of the country, we have been navigating uncharted waters and caring for those most at risk," Harper wrote.
The company had infection control policies in place before COVID-19. Harper said that on Feb. 29, the company implemented additional safeguards, and it kept adding more protections throughout March and April, some even before the CDC or the state recommended them. Each community was responsible for implementing the plan, according to a record from the Georgia Department of Community Health.
Some of the outbreak at Arbor Terrace at Cascade, which happened so early in the U.S. experience of the pandemic, can be attributed to bad luck. But there were other factors that made this place vulnerable.
By early March, employees at Arbor Terrace at Cascade told NPR they were beginning to feel nervous that they did not have enough personal protective equipment for themselves or the residents.
"That's when we really started to ask questions, because we're like, OK, COVID-19 is real," said Heggins, the resident assistant who worked there at the time. "We were asking our staff, like, 'Hey, are there going to be any masks? Are there going to be more gloves? Will we have this protection? Because these are things that they're saying that we need.' "
The CDC had recommended nearly a month earlier that caregivers working with someone they suspected of having the virus should wear PPE or a face mask. But PPE shortages were rampant across the country, and, documents show, Arbor Terrace at Cascade was no different.
In a statement to NPR, Harper acknowledged the difficulties in getting PPE: "Although maintaining adequate PPE was challenging, Arbor Terrace at Cascade never ran out of PPE."
He told NPR that on March 2, the facility began "taking steps to secure PPE beyond the PPE already available at the community. This included purchases from PPE distributors, donations from businesses in the community, and requests to government entities."
According to records from the Georgia Department of Public Health, eight of the 11 Arbor Co. locations in Georgia requested hundreds of N95 respirators, surgical masks, face shields, gowns and gloves between March 13 and 31. None of these orders ended up being fulfilled. A spokesperson for the department told NPR it needed to "prioritize the needs of acute care hospitals." Arbor Terrace at Cascade was one of the three that didn't request any personal protective equipment from the public health department during that two-week time period, although it may have requested PPE from other sources.
"Thankfully, Arbor Terrace had a sufficient supply of PPE prior to and at the start of the novel COVID-19 virus pandemic," Harper wrote.
But on March 27, the day after the first case at the facility was officially reported to the state, the Georgia Department of Public Health reviewed the facility's COVID-19 procedures via a video call. According to an infection prevention assessment obtained by NPR from that review, the department indicated that the facility "has limited masks," and "needs more PPE" for staff to wear consistently when a resident was showing COVID-19 symptoms and when helping residents to perform "high contact activities" such as bathing and dressing. According to the document, the facility reported having staffing issues. By then, the record shows, 15 staff members were showing symptoms of an "ILI," or influenza-like illness.
"There were a lot of times where we would have to go in the rooms without wearing PPE equipment," the staff member who asked not to be named told NPR. "At the end of the day, we weren't just going to leave them by themselves. We still had to take care of them."
That's not what the Arbor Co. was telling families at the time.
On March 26, Harper sent an email to Cascade families, telling them that a resident had tested positive for the coronavirus. He assured families that "all staff members will wear masks and gloves when interacting with all residents."
The next day, the day that the public health department indicated the company "needs more PPE," Harper sent another email: "We have reviewed our processes and procedures with the Georgia Department of Public Health and they have assured us that we are doing what we should be doing in this situation."
The company did keep taking measures to stop the spread of the virus. A disinfecting company conducted a full decontamination of the building on March 27, the day after the first confirmed case. On April 3 and 16, the Georgia National Guard also conducted decontaminations of the facility.
But by then, it was too late.
''That difference can mean life or death''
Not only did the company's missteps at Arbor Terrace at Cascade leave it susceptible to an outbreak, but more systemic factors, such as the facility's population and its location in Atlanta, meant those missteps ultimately proved disastrous.
Assisted living facilities, which are home to about 800,000 mostly older Americans, are especially vulnerable to infectious diseases: You've got a vulnerable population living together with workers coming in and out. Today, nearly 40% of all the U.S. COVID-19 deaths have happened at long-term care facilities such as assisted living facilities, retirement communities and nursing homes.
Arbor Terrace at Cascade was no different. But once the virus was inside the facility, it might have hit those residents harder. African Americans have higher rates of diabetes and high blood pressure, and higher death rates from heart disease. Health disparities such as these have been attributed to systemic racism, and those particular conditions also put individuals at higher risk for severe complications from COVID-19.
Not only that, but a facility surrounded by more cases of the virus matters. One June study found COVID-19 cases in nursing homes across the country are more related to location rather than whether the facility had a poor rating or past infection control violations. Indeed, Arbor Terrace at Cascade had fewer violations per routine inspection than most of the other company locations, according to a database created by The Atlanta Journal-Constitution.
Most of Atlanta is part of Fulton County. That county has about 10% of Georgia's population, but by March 21, it had nearly 20% of the confirmed COVID-19 cases in the state. And within Fulton County, the area near Arbor Terrace at Cascade in southwest Atlanta was hit harder still in the pandemic's early weeks.
There are many reasons why one area might have more COVID-19 cases than another: more people living in crowded housing, using public transportation or who are unable to work from home, among others. Some of those factors are related to poverty, which disproportionately affects people of color. But a New York University study in July of 10 major U.S. metro areas, including Atlanta, found that racial disparities in COVID-19 infections existed beyond disparities related to income.
"When we looked at the early phase of the pandemic within urban U.S. areas, we did not see income explaining away all of the racial and ethnic disparities in COVID outcomes," says Sam Adhikari, who led the NYU study and is an assistant professor of biostatistics at NYU's School of Medicine. "There are other structural systems and historical context that might be putting them at higher risk."
Even a middle-class neighborhood such as Cascade has subtle signs of systemic disinvestment if you look closely. Take home values: Though the median household income of that area is similar to that of Atlanta, the median home value around Cascade is around $120,000 less than Atlanta's median home value.
Nationwide, homes in predominantly Black neighborhoods are worth 23% less than homes in neighborhoods with few or no Black residents, according to research led by Andre Perry, a fellow at the Brookings Institution. The value of your home can help determine the services and resources allocated to your community. It's also a key way to build wealth.
"Many Black neighborhoods simply have less community wealth. And we know that wealth is a protector of sorts, that when we have these economic or health crises, wealth enables us to shelter more," Perry says. "Racism transcends class. Middle-class Black neighborhoods are treated differently than middle-class white neighborhoods. And that difference can mean life or death."
''Can you imagine what happens when a pandemic hits?''
In an email to Cascade families on April 17, Harper wrote: "Many of you have asked why Arbor Terrace Cascade experienced these results. We wish we could tell you. Our protocols and processes are exactly the same in all of our senior living communities."
NPR could not confirm whether the company's protocols, pandemic-related or otherwise, were indeed the same across all its communities, but former Cascade staff members told NPR that Arbor Terrace at Cascade was simply not as nice as the other Arbor Co. locations.
Part of that stems from the age of the community: Most of the other Arbor Co. locations in Georgia were opened or renovated more than a decade after Arbor Terrace at Cascade first opened.
"The building is 20 years old. So how do you compare that to a 6-year-old building?" a former wellness director at the facility, who asked not to be named, told NPR. "Everything about the experience is going to be different."
That staff member added that they believed the company's standards were still the same. But other former staff members disagreed.
"We wouldn't get new stuff. We would get gently used or something that another site didn't want," said Davis, the former maintenance director. "We had to fight for everything we got. Like, we had to pull out a full dissertation of why we should have these things."
He specifically remembered a flight organized by the Arbor Co. for military veterans from several of its facilities that he recalled happening in late 2016 or early 2017. The group from Cascade pulled up in its van to the airfield to meet the groups from the other locations.
"Everybody else's van pulled up. Nice, clean. No problem. And we pull up in this raggedy van," Davis said. "On the side, it had Arbor Terrace at Cascade, but it had bubbles where the paint was peeling off and when it rained, the water came inside, like it was a bucket."
Davis said Harper, the president, acknowledged that they needed to get the van replaced. The company confirmed to NPR that a new van was purchased for the facility in 2016.
"All of a sudden because he's embarrassed now, he was forced to go and get it done. So they did give us money," Davis said. "You can imagine if we're coming to that event ... how bad it had to look."
Davis recalled another incident, when the remnants of Hurricane Irma hit in September 2017.
"I remember it like yesterday. The hurricane was coming. We'd been asking for generators for years. We need generators. We need generators. And they'd never approve that," Davis said.
Cascade's power went out for two days, Davis said. Once the sun went down, he said staff put glow sticks around the residents' necks. Eventually, he said the corporate office brought them gas-powered generators to string up some lights.
"The other Arbor Terraces, they already had generators and they were fully functional and there were no issues," Davis said.
The company confirmed that it has purchased portable generators during storm-related power outages but did not confirm that the other Georgia locations had generators before Arbor Terrace at Cascade.
"The only reason we were not prepared is because we didn't have the funding to be prepared," Davis said. "But as a company, your job is to see where something has a deficit and try to help them navigate through that and not just say, 'Well, you just can't afford it because you don't have enough revenue coming in.' "
In his statement to NPR, Harper did not acknowledge any differences in budgets between the locations but did confirm that each community has its own budget and "funds are not commingled with other Arbor communities."
Of course, any budget differences that did exist between the facilities wouldn't necessarily add up to a higher likelihood of a virus outbreak.
"But if you're always shortchanging something, if you're always the last to be part of something, you can't help but to fail," Davis said. "Can you imagine what happens when a pandemic hits? You get the response that you have."
In his statement to NPR, Harper wrote: "In 1999, we opened Arbor Terrace at Cascade as a state-of-the-art community. We maintain the campus with vigor. ... Arbor Terrace at Cascade is very comparable to other communities of the same age. However, what's most important to note is the care we provide. We have a 21-year history of quality care for this community."
''You can't celebrate their life the way it needs to be''
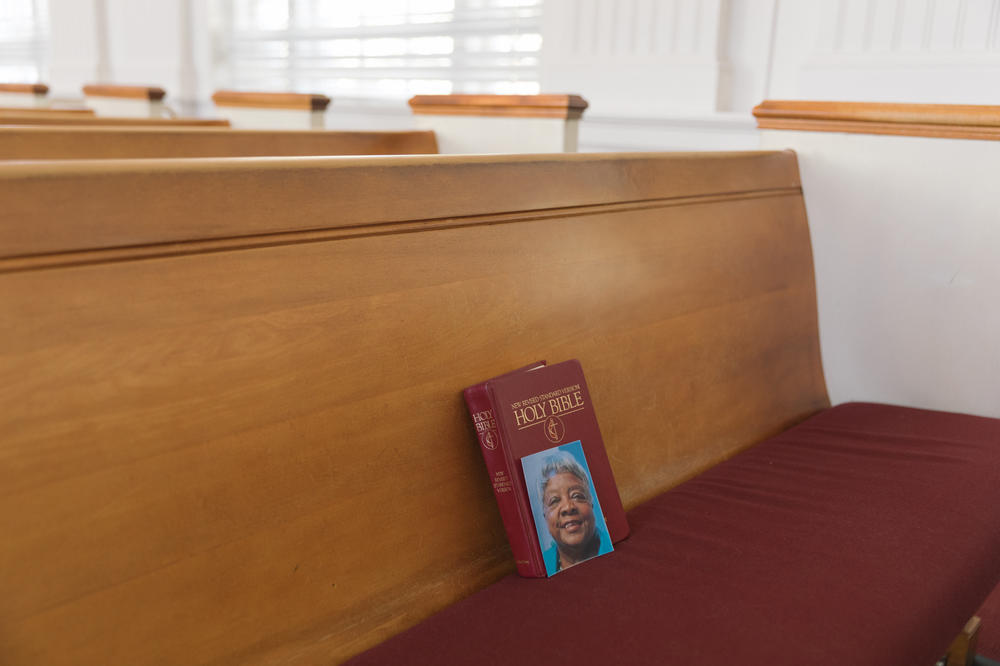
On April 6, Mann's family held a graveside service for her at Westview Cemetery in Atlanta, a short drive from Arbor Terrace at Cascade, where the coronavirus outbreak was still ongoing. Her pastor, Gary Dean, gave a short sermon.
Dean has presided so far over 10 funerals for people who died from the virus, including Ernestine's sister, Carolyn Harris, who died from COVID-19 just six days after Ernestine, and several others from the Arbor Terrace at Cascade outbreak.
"I just feel so bad for all of them because you can't celebrate their life the way it needs to be," Dean said.
Mann's funeral took place on a bright, sunny day. Her family stood by her casket under a green tent. McKinney's husband, Jeff, sang a hymn. They passed out white roses and released a dove.
Because of the pandemic, the funeral was planned to be family only. Otherwise, Dean said, Mann's funeral "would have been standing room only" with family, friends, her sorority sisters from Spelman College, her church community and, of course, the many students she taught across three decades.
Still, a few dozen people had gathered, standing outside their cars or at a distance among the gravestones. And at least one former student was there: the undertaker, representing the many other lives Mann had touched.
Dean told family members they would be all right. He talked about the life Mann lived, and he told the family to be ready.
"This day is going to come for all of us, be it by way of COVID, be it by way of accident or heart attack," he told them and then turned to the Bible: "We have to be ready because we don't know the day nor the hour when it might come."
But there's another kind of readiness, a more secular one, learned from past mistakes.
"We're seeing this time and time again. Not just in this current moment, but the housing crisis, guess who suffered more? Hurricane Katrina, guess who suffered more? Now COVID, guess who's suffering more now?" Perry of the Brookings Institution said. "There will be another disaster that's inevitable."
The question, he said, is who will suffer more the next time.
Copyright 2020 NPR. To see more, visit https://www.npr.org.